A gastric bypass diet is a crucial part of the post-surgery care for individuals who have undergone gastric bypass surgery. The diet is typically divided into several stages, starting with a liquid diet immediately after surgery and gradually progressing to pureed, soft, and eventually solid foods. During the initial phase, patients consume clear liquids such as water, broth, and sugar-free gelatin to stay hydrated and allow the stomach to heal. As the healing progresses, the diet transitions to pureed foods like blended meats, vegetables, and fruits, providing necessary nutrients while still being gentle on the digestive system.
What is the role of diet in gastric bypass?
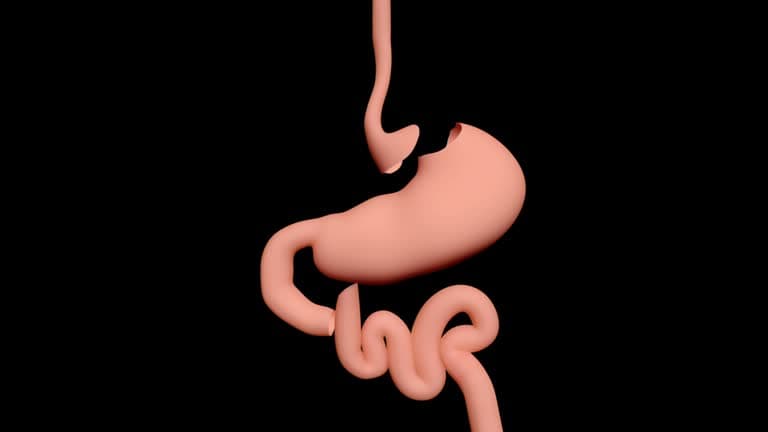
The role of diet in gastric bypass is paramount to the success of the surgery and the long-term health of the patient. Gastric bypass surgery, a form of bariatric surgery, alters the digestive system by creating a small pouch at the top of the stomach and connecting it directly to the small intestine. This not only significantly reduces the stomach's capacity but also alters the absorption process of nutrients. Consequently, the diet following gastric bypass surgery must be carefully managed to support recovery, ensure adequate nutrition, and promote sustainable weight loss.
Immediately after surgery, the diet is strictly controlled, starting with clear liquids to allow the stomach to heal without being overstressed. This phase includes water, broth, and sugar-free gelatin. As the healing progresses, the patient gradually transitions to a full liquid diet, incorporating protein shakes and other nutrient-dense liquids. This is followed by the pureed food stage, where all foods must be blended to a smooth consistency to avoid irritating the digestive system. The primary focus during these stages is on hydration and protein intake, as protein is crucial for healing and maintaining muscle mass.
As patients move into the soft foods stage, they can begin to incorporate more texture into their diet with easily chewable foods like cooked vegetables, soft fruits, and tender meats. This gradual progression helps the digestive system adjust to more substantial foods without causing discomfort or complications. Ultimately, the patient reaches the solid foods stage, where a balanced diet of small, nutrient-dense meals becomes the norm.
Throughout this journey, certain dietary guidelines are essential. High-protein, low-fat, and low-sugar foods are prioritized to support weight loss and overall health. Foods and beverages high in sugar and fat can lead to dumping syndrome, a condition where food moves too quickly through the digestive system, causing nausea, dizziness, and abdominal pain. Additionally, patients are advised to eat smaller, more frequent meals to accommodate the reduced stomach size and to chew food thoroughly to aid digestion.
Vitamin and mineral supplements are often necessary to prevent deficiencies due to the altered absorption process. Common supplements include vitamin B12, iron, calcium, and vitamin D. Regular follow-up with a healthcare provider or a registered dietitian is crucial to monitor nutritional status and make necessary adjustments to the diet.

Diet before gastric bypass
Preparing for gastric bypass surgery involves making significant dietary changes to ensure a successful procedure and promote optimal recovery. The pre-operative diet is designed to shrink the liver, reduce abdominal fat, and improve overall health, making the surgery safer and more effective. This period typically spans two weeks before the surgery, but the exact duration may vary based on individual circumstances and the surgeon's recommendations.
The primary focus of the pre-operative diet is to reduce calorie intake while providing adequate nutrition. High-protein, low-carbohydrate, and low-fat foods are emphasized to promote liver shrinkage and weight loss. Protein is particularly important as it helps maintain muscle mass and supports the healing process. Common protein sources include lean meats, fish, eggs, tofu, and low-fat dairy products. Patients are usually advised to consume protein shakes or supplements to meet their daily protein requirements.
Carbohydrate intake is significantly reduced to minimize the production of glycogen and fat storage in the liver. Simple carbohydrates, such as sugars and refined grains, are strictly limited or eliminated. Instead, patients are encouraged to consume complex carbohydrates found in vegetables, whole grains, and legumes, which provide essential nutrients and fiber.
Hydration is another crucial aspect of the pre-operative diet. Patients are advised to drink plenty of water throughout the day, aiming for at least 64 ounces (about 2 liters) daily. Sugary drinks, carbonated beverages, and alcohol are avoided to prevent unnecessary calorie intake and dehydration.
Portion control and meal timing are essential to prepare the body for the smaller meal sizes required post-surgery. Patients are encouraged to eat smaller, more frequent meals, typically 5-6 times a day, to maintain steady blood sugar levels and avoid overeating. Chewing food thoroughly and eating slowly are also important practices to adopt before surgery, as they will be crucial in the post-operative phase.
In addition to dietary changes, patients are often required to take vitamin and mineral supplements to prevent deficiencies. Common supplements include multivitamins, calcium, vitamin D, and iron. These supplements help ensure that the body receives essential nutrients despite the reduced food intake.
Diet after gastric bypass
The diet after gastric bypass surgery is a crucial component of the recovery process and long-term success of the procedure. This specialized diet is designed to help the stomach heal, promote weight loss, and ensure adequate nutrition. The post-operative diet is typically divided into several stages, each with specific guidelines to accommodate the changes in the digestive system and to gradually reintroduce more solid foods.
Stage 1: Liquid diet
The liquid diet phase is the first stage of the post-operative diet after gastric bypass surgery. This stage typically lasts for about one to two weeks and is designed to allow the stomach to heal without being overstressed. During this period, patients consume only clear liquids to ensure adequate hydration and provide minimal strain on the digestive system.
Clear liquids include water, broth, sugar-free gelatin, and decaffeinated beverages like tea. The goal is to keep the patient hydrated while gradually introducing small amounts of nutrients. Patients are advised to sip slowly and avoid gulping to prevent discomfort. It is essential to drink enough fluids to stay hydrated, aiming for at least 64 ounces (about 2 liters) per day.
As the stomach heals, patients can gradually introduce more nutrient-dense liquids, such as protein shakes, to help meet their protein needs and support recovery. High-protein liquids are crucial during this stage to maintain muscle mass and promote healing.

Stage 2: Pureed diet
The pureed diet phase, follows the liquid diet phase after gastric bypass surgery and typically lasts for about two to four weeks. This stage is crucial for transitioning the patient from a completely liquid diet to more substantial foods while still being gentle on the healing stomach. During the pureed diet phase, all foods must be blended to a smooth, pudding-like consistency to avoid irritation to the digestive system.
Patients are encouraged to consume high-protein foods to support healing and maintain muscle mass. Examples of suitable pureed foods include blended lean meats, poultry, fish, tofu, cooked vegetables, fruits without skins or seeds, and low-fat dairy products. Protein shakes can continue to be a significant part of the diet to ensure adequate protein intake. It is important to eat small, frequent meals—usually five to six times a day—to accommodate the reduced stomach size and prevent discomfort. Patients should also focus on eating slowly, taking small bites, and chewing food thoroughly, even though it is already blended.
Staying hydrated remains essential, and patients should aim to drink at least 64 ounces (about 2 liters) of fluids daily, avoiding sugary or carbonated beverages. Adhering to the pureed diet guidelines helps promote healing, provides necessary nutrients, and prepares the digestive system for the subsequent stages of the post-operative diet.

Stage 3: Soft-foods diet
The soft-foods diet phase, follows the pureed diet phase after gastric bypass surgery and typically lasts for several weeks. This stage is designed to further transition patients from blended foods to more substantial textures, while still being gentle on the healing stomach. During the soft-foods phase, patients can introduce easily chewable and digestible foods into their diet.
Suitable soft foods include scrambled eggs, soft fruits like bananas and melons, cooked vegetables, tender meats like chicken or fish, and cottage cheese. The focus remains on high-protein, low-fat, and low-sugar foods to support weight loss and ensure adequate nutrition. Patients should continue to eat small, frequent meals, usually five to six times a day, to accommodate the reduced stomach size and prevent discomfort.
It is important to chew food thoroughly and eat slowly, taking small bites to aid digestion and avoid any potential blockages. Staying hydrated is crucial, with a goal of at least 64 ounces (about 2 liters) of fluids daily, avoiding sugary or carbonated beverages. Adhering to the soft-foods diet guidelines helps patients adjust to more varied textures, promotes healing, and prepares the digestive system for the eventual reintroduction of solid foods in the final stage of the post-operative diet.

Stage 4: Stabilization
The diet stabilization phase, is the final stage of the post-operative diet after gastric bypass surgery. This stage typically begins around eight weeks after surgery and continues for the long term. The goal of this phase is to establish a balanced, sustainable eating plan that supports ongoing weight loss and overall health. During the stabilization phase, patients can reintroduce a wider variety of solid foods into their diet, focusing on nutrient-dense options.
Patients are encouraged to consume lean proteins, such as poultry, fish, beans, and tofu, along with a variety of fruits and vegetables, whole grains, and low-fat dairy products. Portion control is essential, as the reduced stomach size means patients will feel full quickly. Eating smaller, more frequent meals helps manage hunger and maintain energy levels throughout the day. Healthy eating habits, such as chewing food thoroughly, eating slowly, and avoiding foods high in sugar and fat, are crucial to prevent complications like dumping syndrome. Staying hydrated is also important, with a goal of at least 64 ounces (about 2 liters) of fluids daily, avoiding sugary or carbonated beverages.
Vitamin and mineral supplements continue to be necessary to prevent deficiencies, and regular follow-up appointments with healthcare providers or registered dietitians help monitor progress and make any needed adjustments. The diet stabilization phase is key to achieving long-term success and maintaining the benefits of gastric bypass surgery.

Conclusion
The gastric bypass diet is a critical component of the overall success of gastric bypass surgery. It not only aids in the healing process but also ensures that patients receive the necessary nutrients while promoting sustainable weight loss. This carefully structured diet progresses through various stages—starting with clear liquids, moving to pureed foods, then soft foods, and finally stabilizing with solid foods—to gradually reintroduce more substantial textures and maintain proper nutrition. Adhering to the dietary guidelines helps prevent complications, supports long-term health, and allows patients to achieve and maintain their weight loss goals. Regular follow-ups with healthcare providers and dietitians are essential to monitor progress and make necessary adjustments. By committing to the prescribed dietary regimen, patients can enjoy a healthier lifestyle and the full benefits of their gastric bypass surgery.
Read More