Chronic Kidney Disease (CKD) is a long-term condition where the kidneys gradually lose their ability to function properly over months or years. The kidneys play a crucial role in filtering waste and excess fluids from the blood, which are then excreted in the urine.
What is chronic kidney disease?
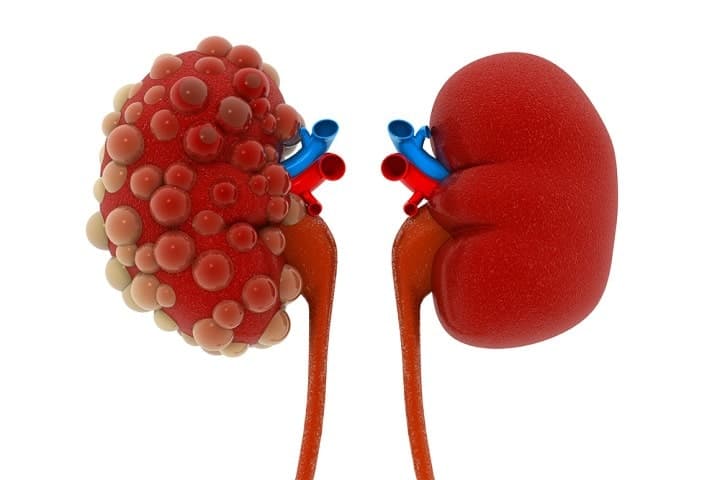
Chronic Kidney Disease (CKD) is a progressive condition characterized by the gradual loss of kidney function over time. The kidneys are vital organs responsible for filtering waste products and excess fluids from the blood, which are then excreted in the urine. When the kidneys are damaged, they lose their ability to perform these essential functions efficiently, leading to a buildup of waste products in the body. CKD is often caused by underlying health conditions such as diabetes and hypertension, which can damage the blood vessels in the kidneys. Other causes include glomerulonephritis, an inflammation of the kidney’s filtering units, and polycystic kidney disease, a genetic disorder that leads to the formation of cysts in the kidneys.
In the early stages of CKD, individuals may not experience noticeable symptoms, making it a silent but serious condition. As the disease progresses, symptoms may include fatigue, weakness, swelling in the feet and ankles, shortness of breath, nausea, vomiting, and high blood pressure. These symptoms occur because the kidneys are no longer able to maintain the body’s balance of fluids, electrolytes, and waste products. Diagnosing CKD typically involves blood tests to measure levels of creatinine and urea, as well as urine tests to check for the presence of protein or blood, which can indicate kidney damage.
Living with CKD requires ongoing medical care and lifestyle adjustments to manage symptoms and prevent complications. Regular monitoring by healthcare professionals is essential to track the progression of the disease and adjust treatment plans as needed. With proper management, individuals with CKD can maintain a good quality of life and reduce the risk of severe complications. Early detection and intervention are key to slowing the progression of CKD and improving outcomes for those affected by this chronic condition.
Signs & Symptoms of chronic kidney disease
In its early stages, CKD often presents no noticeable symptoms, making it a silent but serious condition. As the disease progresses, various signs and symptoms may emerge, reflecting the kidneys’ declining ability to filter waste and excess fluids from the blood.
One of the earliest signs is often an increase in the frequency of urination, particularly at night. Patients may also experience persistent fatigue and weakness due to the buildup of toxins in the blood. Swelling, or edema, in the feet and ankles is common as the kidneys fail to remove excess fluid from the body.
Other symptoms include nausea, vomiting, and a loss of appetite, which can lead to unintended weight loss. High blood pressure, or hypertension, is both a cause and a symptom of CKD, as the kidneys play a crucial role in regulating blood pressure. As kidney function deteriorates, patients may notice changes in their urine, such as blood in the urine (hematuria) or foamy urine, which indicates the presence of protein (proteinuria). Decreased mental sharpness and difficulty concentrating are also reported, likely due to the accumulation of waste products affecting brain function.
Muscle cramps and twitches can occur, often due to electrolyte imbalances caused by impaired kidney function. Persistent itching is another symptom, resulting from the buildup of waste products in the blood. Shortness of breath may develop if fluid accumulates in the lungs, and chest pain can occur if fluid builds up around the lining of the heart. In advanced stages, CKD can lead to severe complications such as cardiovascular disease, anemia, bone disease, and nerve damage.
It’s important to note that these symptoms are often nonspecific and can be attributed to other health conditions, which is why CKD can go undiagnosed until it reaches a more advanced stage. Early intervention and management can slow the progression of CKD and improve the quality of life for those affected.
Causes of kidney disease
Kidney disease can arise from a variety of underlying conditions and factors that impair the kidneys’ ability to function properly.
The most common causes of chronic kidney disease (CKD) are diabetes and high blood pressure. Diabetes, particularly type 1 and type 2, can damage the blood vessels in the kidneys, leading to nephropathy. High blood pressure, or hypertension, exerts excessive force on the blood vessels, including those in the kidneys, which can lead to damage over time. These two conditions are responsible for the majority of CKD cases.
Other significant causes include glomerulonephritis, an inflammation of the kidney’s filtering units (glomeruli), which can result from infections, autoimmune diseases, or other conditions. Polycystic kidney disease (PKD) is a genetic disorder characterized by the growth of numerous cysts in the kidneys, which can impair their function. Lupus nephritis, a complication of the autoimmune disease lupus, occurs when the immune system attacks the kidneys, causing inflammation and damage.
Certain medications and toxins can also lead to kidney damage. Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics, and other nephrotoxic drugs can harm the kidneys. Additionally, exposure to heavy metals and other environmental toxins can contribute to kidney disease. Infections, such as recurrent urinary tract infections (UTIs) or kidney infections (pyelonephritis), can cause scarring and damage to the kidneys over time.
Other risk factors include a family history of kidney disease, which can increase an individual’s susceptibility to developing the condition. Obesity, smoking, and a sedentary lifestyle are also linked to an increased risk of CKD. Cardiovascular diseases, such as heart disease and stroke, are closely associated with kidney disease, as the health of the heart and kidneys are interdependent. Conditions like obstructive uropathy, where urine flow is blocked, can lead to kidney damage if not treated promptly.
In some cases, kidney disease can result from congenital abnormalities that affect kidney structure and function from birth. Aging is another factor, as kidney function naturally declines with age, making older adults more susceptible to CKD. Early detection and management of these underlying causes are crucial in preventing the progression of kidney disease and maintaining overall kidney health.
The 5 stages of chronic kidney disease
Chronic Kidney Disease (CKD) is categorized into five stages based on the estimated glomerular filtration rate (eGFR), which measures how well the kidneys filter waste from the blood.
Stage 1 CKD is characterized by a normal or high eGFR (90 mL/min or higher) but with evidence of kidney damage, such as protein in the urine. At this stage, the kidneys are still functioning well, and symptoms are usually absent.
Stage 2 CKD involves a mild decrease in eGFR (60-89 mL/min) with signs of kidney damage. Like Stage 1, symptoms are often minimal, but early intervention can help slow disease progression.
Stage 3 CKD is divided into two substages: 3a (eGFR 45-59 mL/min) and 3b (eGFR 30-44 mL/min). At this stage, kidney function is moderately reduced, and symptoms such as fatigue, swelling in the extremities, and changes in urination patterns may begin to appear. Patients may also experience high blood pressure and bone disease due to the kidneys’ reduced ability to maintain electrolyte balance and remove waste.
Stage 4 CKD is marked by a severe reduction in eGFR (15-29 mL/min). Symptoms become more pronounced and can include severe fatigue, swelling, shortness of breath, and nausea. At this stage, patients need to prepare for potential kidney replacement therapy, such as dialysis or a kidney transplant, as kidney function continues to decline.
Stage 5 CKD, also known as end-stage renal disease (ESRD), occurs when eGFR falls below 15 mL/min. The kidneys have lost nearly all their ability to function effectively, leading to a dangerous buildup of waste products in the blood. Symptoms are severe and can include persistent nausea, vomiting, loss of appetite, itching, and fluid retention, which can cause swelling and shortness of breath. At this stage, dialysis or a kidney transplant is necessary to sustain life.
Managing CKD at any stage involves controlling underlying conditions like diabetes and hypertension, adhering to a kidney-friendly diet, and regular monitoring by healthcare professionals to slow disease progression and improve quality of life.

The complications of chronic kidney disease
Chronic Kidney Disease (CKD) can lead to a range of serious complications as the kidneys lose their ability to filter waste and maintain the body’s chemical balance.
One of the most common complications is anemia, which occurs when the kidneys fail to produce enough erythropoietin, a hormone that stimulates red blood cell production. This can result in fatigue, weakness, and shortness of breath.
Bone disease is another significant complication, as impaired kidney function disrupts the balance of calcium and phosphorus in the body, leading to weakened bones and an increased risk of fractures.
Cardiovascular disease is closely linked to CKD, with patients at a higher risk of heart attacks, strokes, and heart failure due to the increased strain on the cardiovascular system from high blood pressure and fluid overload.
Fluid retention is a common issue, causing swelling in the legs, ankles, and feet, and can lead to pulmonary edema, where fluid accumulates in the lungs, causing shortness of breath.
Hyperkalemia, or high potassium levels, can develop as the kidneys lose their ability to excrete potassium, leading to dangerous heart rhythm problems.
Metabolic acidosis is another complication, where the kidneys cannot remove enough acid from the blood, resulting in a chemical imbalance that can cause muscle wasting and bone disease.
High blood pressure (hypertension) is both a cause and a consequence of CKD. As kidney function declines, the kidneys release more renin, a hormone that raises blood pressure, creating a vicious cycle that further damages the kidneys.
Nerve damage (neuropathy) can also occur, leading to symptoms such as tingling, numbness, and pain in the hands and feet.
Gout, a form of arthritis, can develop due to the accumulation of uric acid crystals in the joints, causing severe pain and inflammation.
Nutritional deficiencies are common in CKD patients, as the disease affects the body’s ability to absorb and utilize nutrients. This can lead to weight loss, muscle wasting, and general weakness.
Infections are more likely due to a weakened immune system, making patients more susceptible to illnesses.
Sleep disturbances, including insomnia and restless legs syndrome, are also prevalent among CKD patients, further impacting their quality of life.
Managing these complications requires a comprehensive approach, including medication, dietary changes, and regular monitoring by healthcare professionals.

How is kidney disease diagnosed?
Diagnosing kidney disease involves a series of tests and evaluations to determine the extent of kidney damage and identify the underlying cause. The process typically begins with a thorough review of the patient’s medical history and a physical examination. The doctor will inquire about any symptoms, family history of kidney disease, and risk factors such as diabetes, high blood pressure, or use of medications that could affect kidney function.
Blood tests are crucial in diagnosing kidney disease. The most common test is the measurement of serum creatinine levels, a waste product that the kidneys normally filter out of the blood. Elevated creatinine levels indicate impaired kidney function.
Another important test is the glomerular filtration rate (GFR), which estimates how well the kidneys are filtering blood. A GFR below 60 mL/min/1.73 m² for three months or more is indicative of chronic kidney disease. Blood urea nitrogen (BUN) levels are also measured, as high levels can suggest reduced kidney function.
Urine tests are equally important in diagnosing kidney disease. A urinalysis can detect abnormalities such as protein (proteinuria) or blood (hematuria) in the urine, which are signs of kidney damage. The presence of albumin, a type of protein, in the urine is particularly significant and can be detected through a urine albumin-to-creatinine ratio (UACR) test. Persistent proteinuria is a hallmark of chronic kidney disease.
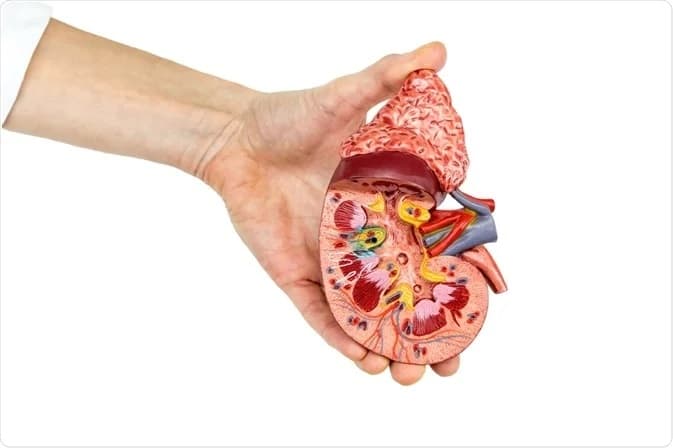
Imaging tests provide visual information about the kidneys’ structure and size. Ultrasound is commonly used to detect any structural abnormalities, such as cysts, tumors, or obstructions. In some cases, a CT scan or MRI may be performed to get a more detailed view of the kidneys and surrounding tissues.
Kidney biopsy is a procedure where a small sample of kidney tissue is removed and examined under a microscope. This test is often done when the cause of kidney disease is unclear or when a specific diagnosis is needed to guide treatment. The biopsy can reveal the extent of kidney damage and help identify conditions such as glomerulonephritis or interstitial nephritis.
Overall, diagnosing kidney disease is a comprehensive process that combines medical history, physical examination, and a variety of tests to accurately assess kidney function and determine the underlying cause.
How is chronic kidney disease treated?
Chronic Kidney Disease (CKD) treatment focuses on slowing the progression of the disease, managing symptoms, and preventing complications. The primary approach involves addressing the underlying causes, such as diabetes and high blood pressure. For patients with diabetes, maintaining optimal blood sugar levels through medication, diet, and lifestyle changes is crucial. Similarly, controlling high blood pressure with antihypertensive medications, such as ACE inhibitors or ARBs, can help protect kidney function.
Dietary modifications play a significant role in managing CKD. Patients are often advised to follow a low-protein diet to reduce the kidneys’ workload and minimize waste product buildup in the blood. Limiting salt intake helps control blood pressure and reduce fluid retention, while managing potassium and phosphorus levels is essential to prevent complications like hyperkalemia and bone disease.
Medications are also used to treat complications associated with CKD. For instance, erythropoiesis-stimulating agents (ESAs) can help manage anemia by stimulating red blood cell production. Phosphate binders are prescribed to control high phosphorus levels, and vitamin D supplements may be necessary to maintain bone health. Diuretics can help reduce fluid retention and swelling, while statins are often used to manage high cholesterol levels, reducing the risk of cardiovascular disease.
In advanced stages of CKD, when kidney function is severely impaired, renal replacement therapy becomes necessary. Dialysis is a common treatment option that involves using a machine to filter waste products and excess fluids from the blood. There are two main types of dialysis: hemodialysis, which is typically performed in a clinic, and peritoneal dialysis, which can be done at home. Dialysis helps manage symptoms and prolongs life, but it does not cure CKD.
Kidney transplantation is another treatment option for end-stage renal disease (ESRD). This involves surgically placing a healthy kidney from a donor into the patient’s body. A successful transplant can significantly improve the quality of life and eliminate the need for dialysis. However, patients must take immunosuppressive medications for life to prevent the body from rejecting the new kidney.
Overall, managing CKD requires a comprehensive approach that includes medical treatment, lifestyle changes, and regular monitoring by healthcare professionals.

Conclusion
In conclusion, chronic kidney disease (CKD) is a progressive condition that significantly impacts the kidneys’ ability to filter waste and maintain the body’s chemical balance. Early detection and management are crucial in slowing the progression of the disease and preventing severe complications. By addressing underlying causes such as diabetes and hypertension, making dietary and lifestyle changes, and adhering to prescribed treatments, individuals with CKD can maintain a better quality of life. Regular monitoring and proactive healthcare can help manage symptoms and improve outcomes.
Read More