Female sterilization procedures are permanent methods of birth control designed to prevent pregnancy. These procedures involve blocking, sealing, or cutting the fallopian tubes to prevent eggs from traveling from the ovaries to the uterus. By disrupting the pathway for the eggs, fertilization by sperm becomes impossible, effectively providing long-term contraception.
What is female sterilization?
Female sterilization is a permanent method of contraception designed to prevent pregnancy by blocking or sealing the fallopian tubes. The fallopian tubes are the pathways through which eggs travel from the ovaries to the uterus. By disrupting this pathway, female sterilization ensures that eggs cannot meet sperm, thereby preventing fertilization and pregnancy. This procedure is typically chosen by women who are certain they do not want to have any more children or who wish to avoid the risks and side effects associated with other forms of contraception. There are several techniques for female sterilization, with tubal ligation being the most common.
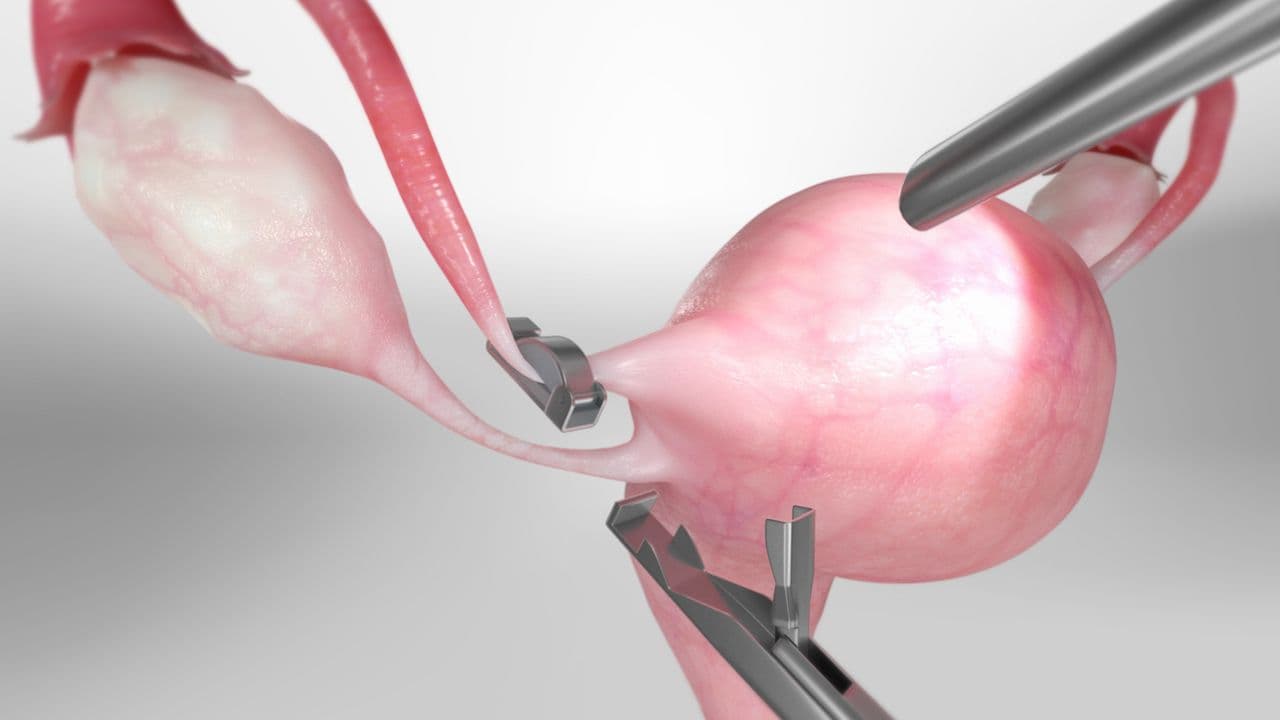
Tubal ligation, often referred to as “having one's tubes tied”, involves surgically cutting, sealing, or blocking the fallopian tubes. This can be done using various methods, such as applying clips or rings, or by cauterizing (burning) the tubes. The procedure can be performed through a small incision in the abdomen using laparoscopic instruments, or during a cesarean section if the woman is already undergoing surgery.
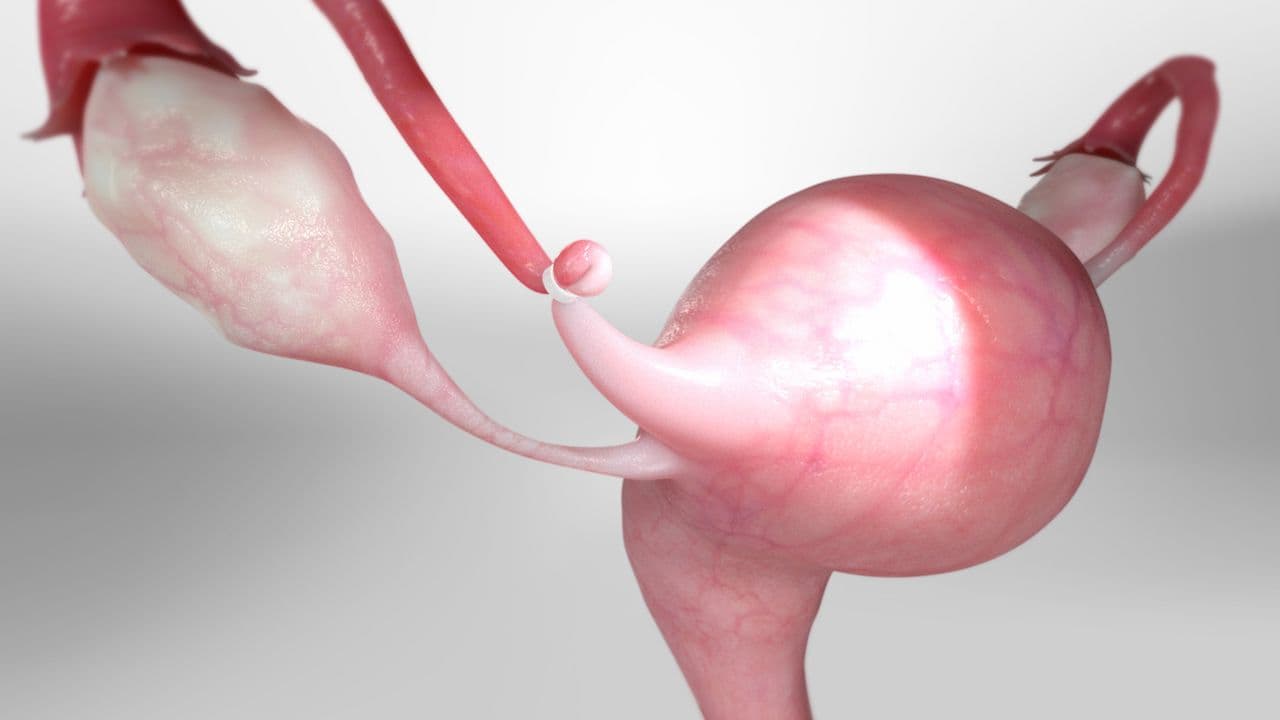
Another method is salpingectomy, which involves the complete removal of the fallopian tubes. This technique is gaining popularity due to its additional health benefits, such as reducing the risk of ovarian cancer. Unlike tubal ligation, which may occasionally fail due to the tubes potentially rejoining, salpingectomy offers a more definitive solution.
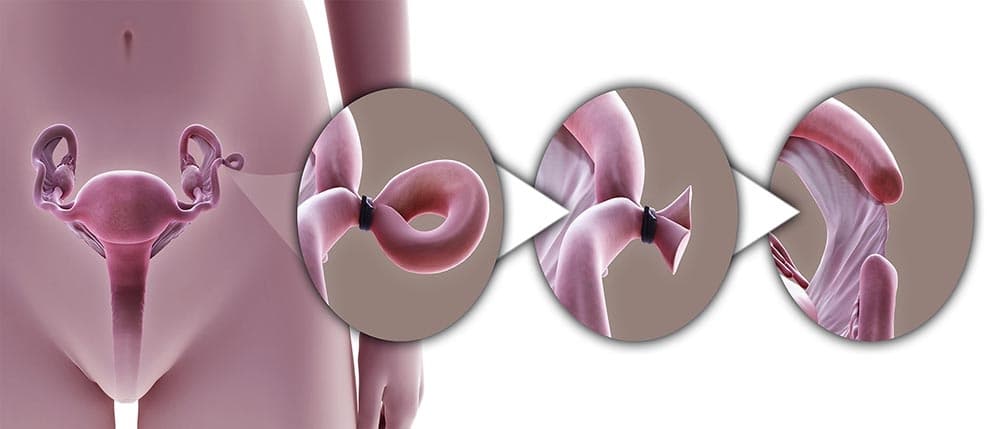
Hysteroscopic sterilization, a non-surgical method, involves inserting a small device into the fallopian tubes through the cervix. The device causes scar tissue to form, which eventually blocks the tubes. However, this method has become less common due to concerns about its long-term effectiveness and potential complications.
Female sterilization procedures are typically performed in a hospital or outpatient surgical center, often under general or local anesthesia. The recovery time varies depending on the specific technique used, but most women can resume normal activities within a few days to a week. It is essential for women to consider the permanent nature of sterilization and discuss all available options with their healthcare provider before undergoing the procedure. It is important to note that female sterilization does not protect against sexually transmitted infections (STIs), so the use of barrier methods, such as condoms, may still be necessary for STI prevention.
How is female sterilization performed?
Female sterilization is performed through two primary methods: tubal ligation and nonsurgical sterilization. Both techniques aim to prevent pregnancy permanently by blocking or sealing the fallopian tubes, thus preventing the eggs from traveling from the ovaries to the uterus.
Tubal Ligation: Tubal ligation, often referred to as “having one's tubes tied”, is a surgical procedure that involves cutting, sealing, or blocking the fallopian tubes. This can be achieved through various techniques, such as using clips, rings, or by cauterizing (burning) the tubes. The procedure can be performed through a small incision in the abdomen, known as laparoscopic tubal ligation, or during a cesarean section if the woman is already undergoing surgery. In a laparoscopic tubal ligation, the surgeon inserts a laparoscope (a thin, lighted tube with a camera) and specialized surgical instruments through small incisions in the abdomen. The laparoscope allows the surgeon to visualize the fallopian tubes and perform the procedure with precision. Tubal ligation is usually performed under general anesthesia, and most women can go home the same day. Recovery time varies, but most patients can resume normal activities within a few days to a week.
Nonsurgical Sterilization: Nonsurgical sterilization, such as hysteroscopic sterilization, involves inserting a small device into the fallopian tubes through the cervix. The procedure does not require any incisions and is typically performed under local anesthesia or sedation. A hysteroscope (a thin, lighted tube with a camera) is used to guide the insertion of the device. Once in place, the device causes scar tissue to form, which eventually blocks the fallopian tubes and prevents eggs from reaching the uterus. This method is less invasive than tubal ligation and usually has a shorter recovery time. However, it has become less common due to concerns about its long-term effectiveness and potential complications.
Both tubal ligation and nonsurgical sterilization are highly effective methods of permanent contraception. However, they are considered irreversible, so it is essential for women to carefully consider their decision and discuss all available options with their healthcare provider before undergoing sterilization. Additionally, these procedures do not protect against sexually transmitted infections (STIs), so the use of barrier methods, such as condoms, may still be necessary for STI prevention.

Recovery from female sterilization
Recovering from female sterilization, whether through tubal ligation or nonsurgical methods, typically involves a period of rest, careful monitoring, and gradual return to normal activities. The recovery process varies depending on the specific technique used, the patient's overall health, and the individual’s response to the procedure.
Post-Tubal Ligation Recovery: For those who undergo tubal ligation, the procedure is often performed on an outpatient basis, meaning patients can return home the same day. After the surgery, it is common to experience some discomfort, pain, or cramping in the abdominal area, as well as potential shoulder pain caused by the gas used to inflate the abdomen during the laparoscopic procedure. Pain medications are typically prescribed to manage these symptoms. It is essential to avoid strenuous activities, heavy lifting, and intense exercise for at least one to two weeks to allow the incision sites to heal properly. Most women can return to their normal daily activities, including work, within a few days to a week, although complete recovery may take a little longer.
Post-Nonsurgical Sterilization Recovery: Recovery from nonsurgical sterilization methods, such as hysteroscopic sterilization, is generally shorter and less intense. Since there are no incisions involved, patients may experience less pain and discomfort. The most common symptoms include mild cramping, vaginal bleeding, and discharge for a few days following the procedure. Over-the-counter pain relievers can help manage any discomfort. Most women can resume their normal activities within a day or two, but it is essential to follow the healthcare provider's instructions and attend any scheduled follow-up appointments to ensure the procedure's success.
Regardless of the sterilization method, it is crucial to monitor for any signs of complications, such as excessive bleeding, infection, severe pain, or fever. Patients should contact their healthcare provider if they experience any unusual symptoms. Additionally, it is important to avoid sexual intercourse, using tampons, and douching for a specified period, as advised by the healthcare provider, to reduce the risk of infection and allow the body to heal.
What are the benefits of female sterilization?
Female sterilization offers several benefits, making it an attractive option for many women seeking permanent contraception.
One of the primary advantages is its high effectiveness in preventing pregnancy. Once the procedure is successfully performed, the chances of becoming pregnant are extremely low, providing long-term peace of mind for women who are certain they do not want to have any more children. Unlike other forms of contraception that require ongoing attention, such as daily pills, monthly injections, or the use of barrier methods, female sterilization is a one-time procedure that eliminates the need for continuous contraceptive management.
Another significant benefit is the convenience and freedom it offers. Women who undergo sterilization no longer need to worry about the possibility of unintended pregnancies, allowing them to focus on other aspects of their lives without the burden of contraceptive routines. This can be particularly advantageous for women who may have difficulty adhering to regular contraceptive schedules or who experience side effects from hormonal birth control methods.
Female sterilization also allows women to avoid the hormonal fluctuations and potential side effects associated with hormonal contraceptives, such as mood swings, weight gain, and increased risk of certain health conditions. For women who cannot use hormonal methods due to medical reasons, sterilization provides a reliable and hormone-free alternative.
Additionally, female sterilization can have positive effects on a woman's sexual health and relationship. Without the need for ongoing contraception, couples can enjoy a more spontaneous and worry-free sexual experience. This can lead to increased sexual satisfaction and improved intimacy within relationships.
Furthermore, sterilization procedures such as salpingectomy offer additional health benefits, such as reducing the risk of ovarian cancer. This added advantage makes the procedure appealing to women who are at higher risk for this type of cancer.

What are the disadvantages of female sterilization?
While female sterilization offers numerous benefits, it also comes with several disadvantages that women should consider before opting for this permanent method of contraception.
One of the primary disadvantages is its irreversible nature. Once the procedure is performed, it is extremely difficult, if not impossible, to reverse. This means that women who undergo sterilization must be absolutely certain that they do not wish to have any more children in the future. Changes in life circumstances, such as remarriage or the loss of a child, may lead to regret and a desire to reverse the procedure, which may not be feasible.
Another disadvantage is the potential for surgical complications. Like any surgical procedure, female sterilization carries risks such as infection, bleeding, and adverse reactions to anesthesia. While these complications are relatively rare, they can occur and may require additional medical intervention. Tubal ligation, in particular, involves making incisions in the abdomen, which can lead to longer recovery times and potential postoperative discomfort.
Female sterilization does not protect against sexually transmitted infections (STIs). Women who undergo sterilization may still need to use barrier methods, such as condoms, to protect themselves and their partners from STIs. This limitation may be a drawback for individuals seeking comprehensive protection from both pregnancy and infections.
Hormonal changes can also be a concern, especially if the sterilization procedure involves the removal of the ovaries (oophorectomy). This can result in immediate menopause, leading to symptoms such as hot flashes, night sweats, mood swings, and an increased risk of osteoporosis and cardiovascular disease. Hormone replacement therapy (HRT) may be necessary to manage these symptoms, which can have its own set of side effects and risks.
Lastly, there is a small risk of sterilization failure. While female sterilization is highly effective, no method is 100% foolproof. In rare cases, the fallopian tubes may heal and rejoin, potentially leading to an unintended pregnancy. If pregnancy occurs after sterilization, there is an increased risk of it being an ectopic pregnancy, where the fertilized egg implants outside the uterus, which can be a medical emergency.
Conclusion
In conclusion, female sterilization procedures offer a highly effective and permanent solution for women seeking long-term contraception. By preventing the eggs from traveling through the fallopian tubes, these procedures ensure that fertilization cannot occur. Whether through surgical methods like tubal ligation and salpingectomy or non-surgical techniques such as hysteroscopic sterilization, each approach provides unique benefits and considerations. However, the irreversible nature of these procedures, along with potential risks and complications, necessitates careful deliberation and thorough discussions with healthcare providers. Women must be certain about their decision and fully understand the implications before opting for sterilization. Ultimately, female sterilization empowers women to take control of their reproductive health, offering them the freedom and peace of mind that comes with reliable, permanent contraception.
Read More