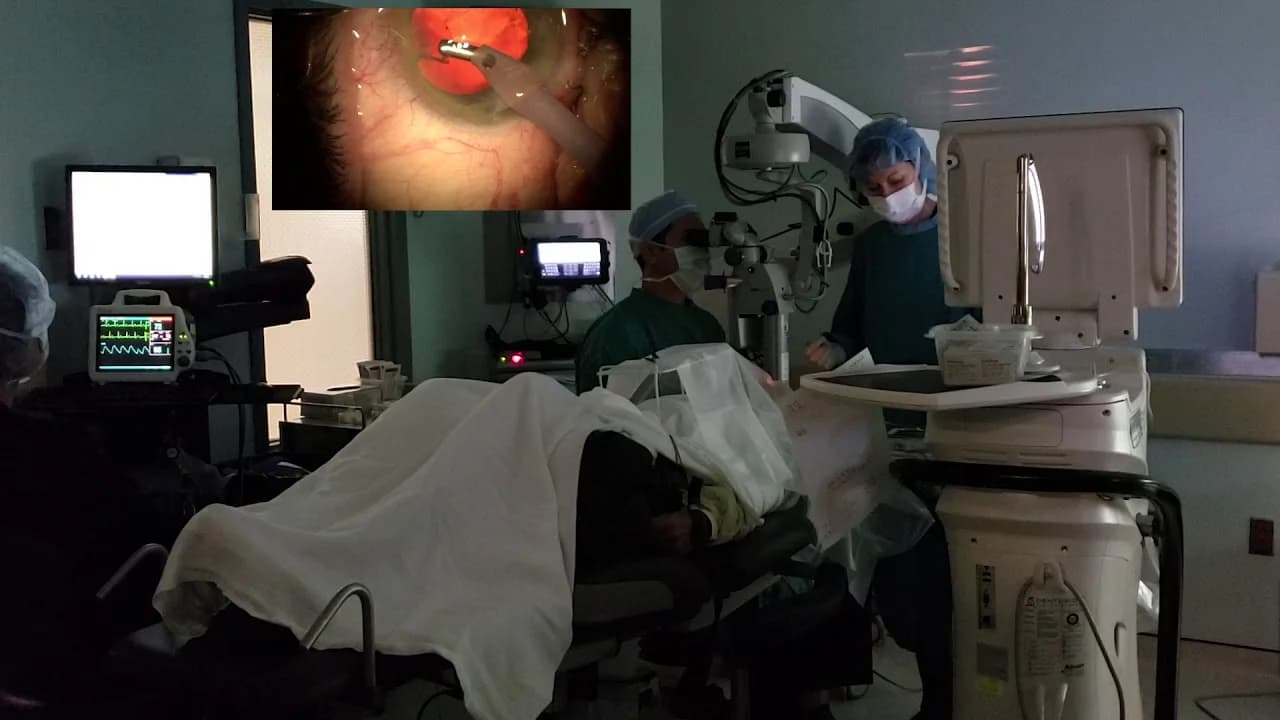
Cataract surgery involves the removal of your eye lens and replacing it with an artificial lens. Cataract causes your clear eye lens to become cloudy which eventually affects your vision. Since cataract surgery is performed by an ophthalmologist on an outpatient basis, you won’t need to stay in the hospital after the surgery. This is a very common and safe procedure.
Why cataract surgery?
Cataract surgery is performed to treat cataracts. Cataracts can cause blurry vision and increase the glare from lights. In situations where a cataract is causing difficulties with your normal activities, cataract surgery is suggested. In most cases, waiting to have cataract surgery won't harm your eye, so you have time to consider your options. If your vision is still quite good, you may not need cataract surgery for many years, if ever.

What are the risks of cataract surgery?
Inflammation
Infection
Bleeding
Swelling
Drooping eyelid
Dislocation of artificial lens
Retinal detachment
Glaucoma
Secondary cataract
Loss of vision
Your risk of complications is greater if you have another eye disease or a serious medical condition. In patients suffering from underlying eye damage such as glaucoma or muscular degeneration, cataract surgery may fail to improve vision. So you should treat other eye problems before deciding to have cataract surgery.

What are cataract surgery complications?
Complications can occur during any surgical procedure. With cataract surgery, several specific complications will be on your surgeon’s radar.
Pain: Pain is an expected complication of most surgical procedures. Since cataract surgery involves only the superficial layers of your eye, over-the-counter pain relievers will generally help.
Bleeding: Hemorrhage can occur in people with diabetes, high blood pressure, or other existing conditions after cataract surgery.
Infection: Most procedures carry some risk of infection from surgical tools, the surgeon’s technique, or wound care after surgery.
New or continued vision problems: In some cases, cataract surgery may not be effective, and you may continue to have vision problems or worse vision after surgery.
Floaters: Floaters are the term given to tiny particles of protein or collagen that can cross your field of vision and cast shadows. Floaters don’t always need treatment but can sometimes be a sign of a more serious problem.
Dry or itchy eyes: As the tissue heals, dryness and itching are common. Your eyes may feel itchy, gritty, or dry. Your doctor may suggest lubricating eye drops to help with this problem.
Allergic reactions: The use of general anesthesia for cataract surgery is rare, and usually only in pediatric cases.
Inflammation: When your surgeon makes contact with your eye, a small number of white blood cells or protein may build up in the front chamber of the eye, creating blurred vision or light sensitivity. This condition is usually temporary and can be treated with topical steroids.
Corneal edema: Swelling in the cornea can occur anywhere after surgery, but is usually at incision sites. This condition can be treated with topical steroids that will reduce swelling.
Increased pressure: Up to half of those having cataract surgery will experience some increase in pressure in their eye after the procedure, but pressure levels usually return to normal within 24 hours.
Iris prolapse: In rare cases, surgery could cause trauma to the iris, resulting in a prolapsed iris. This is sometimes related to poor wound closure or healing at incision sites, or long periods of high pressure in the eye.
Retained lens fragments: In some cases, there may be tiny pieces of your natural lens left behind after cataract surgery. These can appear days or even years later in the form of blurry vision, light sensitivity, tearing, and redness. If lens fragments are the culprit, they should be surgically removed, ideally by the original surgeon who performed the procedure.
Posterior capsular opacification: Most common in people who have diabetes or who have had prior eye surgeries, this condition results in the formation of tiny particles trapped in the layer behind the lens.
Cystoid macular edema: This is the most common complication of most cataract surgeries and appears up to 8 weeks after the procedure. It occurs in 1 to 2 percent of all cataract surgeries. Swelling is caused by the buildup of fluid in the eye that can lead to decreased vision.
Intraocular lens dislocation: After cataract surgery, there is a chance that the intraocular lens that replaces the natural lens could shift or move. Blurred vision is a common symptom, and this may have to be repaired surgically.
Retinal detachment: This is a serious complication that occurs mainly in younger patients who have other eye problems or who have had dislocated intraocular lenses. Retinal detachment requires immediate medical care.
Capsular contraction syndrome: The remaining natural lens cells create a fibrous material that contracts, reducing the size of the thin membrane that surrounds the lens.
Chronic corneal edema: This complication can result in chronic irreversible swelling of the cornea.
Risk Factors for Complications
While complications from cataract surgery can happen to anyone, they are more common in some instances:
Those over the age of 60
Those with diabetes
Those who have cataract surgery at the same time as other procedures
Those with other eye disorders, including glaucoma
Those taking certain medications, such as tamsulosin
Conclusion
While cataract surgery is generally considered safe and effective, it’s important to be aware of its potential risks. These include minor complications such as swelling and bleeding, as well as more serious ones like retinal detachment and loss of vision. However, complications are relatively rare and most can be successfully treated. It’s also worth noting that underlying eye conditions can affect the outcome of the surgery. Therefore, a comprehensive eye examination and discussion with your ophthalmologist is crucial before deciding to undergo cataract surgery. This will help ensure that you are fully informed about the potential risks and benefits, and can make an informed decision about your eye health.
Read more: