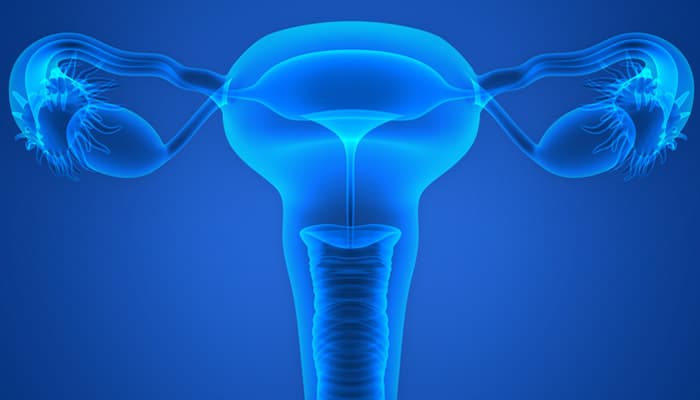
A hysterectomy is a surgical procedure that involves the removal of a woman's uterus. This operation can be performed for various medical reasons, including the treatment of uterine fibroids, endometriosis, chronic pelvic pain, abnormal bleeding, or gynecologic cancers such as cervical, uterine, or ovarian cancer.
Why is Hysterectomy performed?
A hysterectomy is performed for a variety of medical reasons, primarily to address conditions affecting the uterus that cannot be effectively treated with less invasive methods. One of the most common indications for a hysterectomy is the presence of uterine fibroids, which are non-cancerous growths that can cause heavy menstrual bleeding, pelvic pain, and pressure on other organs. In cases where fibroids significantly impact a woman's quality of life and other treatments, such as medications or less invasive procedures, have failed, a hysterectomy may be recommended.
Endometriosis is another condition that may necessitate a hysterectomy. Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterus, causing chronic pain, heavy bleeding, and infertility. When conservative treatments, such as hormonal therapy or laparoscopic surgery, are insufficient in managing the symptoms, a hysterectomy may be considered as a definitive solution.
Chronic pelvic pain, which can be caused by various underlying issues, may also lead to the decision to perform a hysterectomy. If the pain is severe and other treatments have not provided relief, removing the uterus may help alleviate the symptoms and improve the patient's quality of life.
Abnormal uterine bleeding that does not respond to medical treatments is another reason for a hysterectomy. This can include heavy, prolonged, or irregular menstrual bleeding that disrupts a woman's daily activities and overall health. Removing the uterus can effectively resolve this issue when other interventions are not successful.
Gynecologic cancers, such as cervical, uterine, and ovarian cancer, are among the most serious conditions that may require a hysterectomy. In these cases, the surgery is performed to remove cancerous tissues and prevent the spread of the disease. Depending on the stage and type of cancer, a hysterectomy may be part of a broader treatment plan that includes chemotherapy and radiation therapy.
What are the Types of Hysterectomy?
There are several types of hysterectomy, each tailored to the specific needs of the patient and the underlying medical condition. The main types of hysterectomy are as follows.
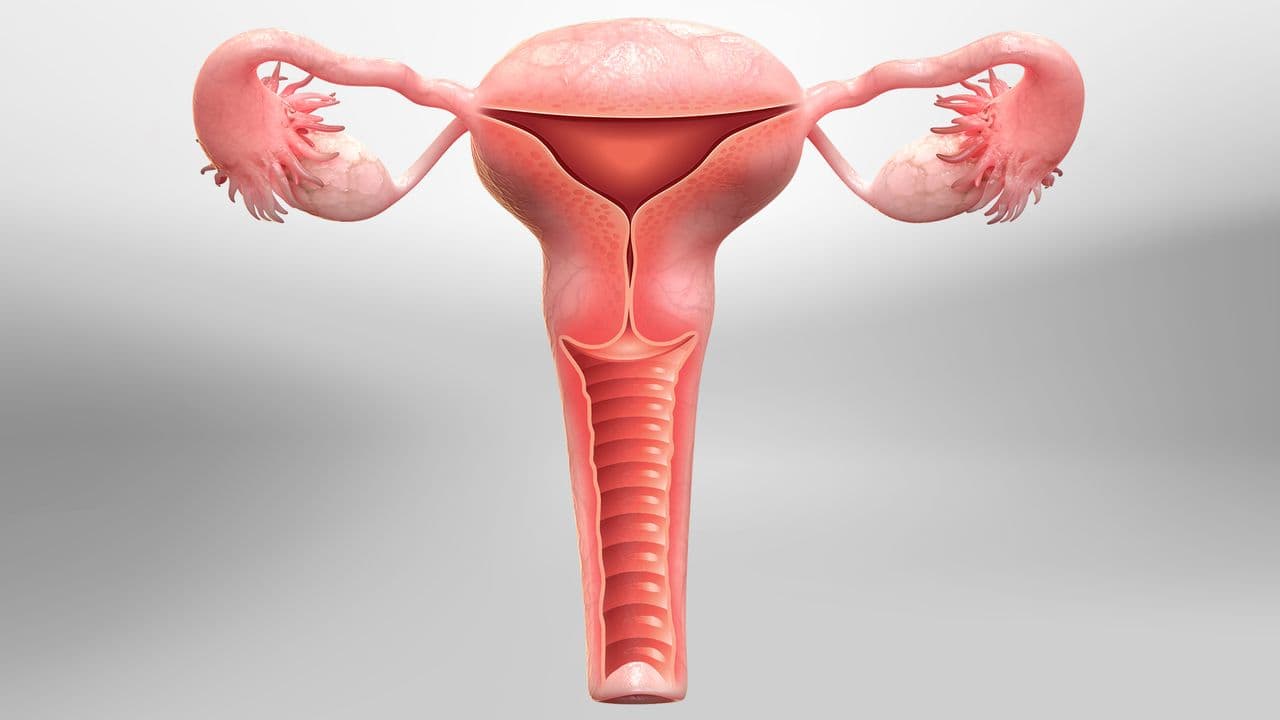
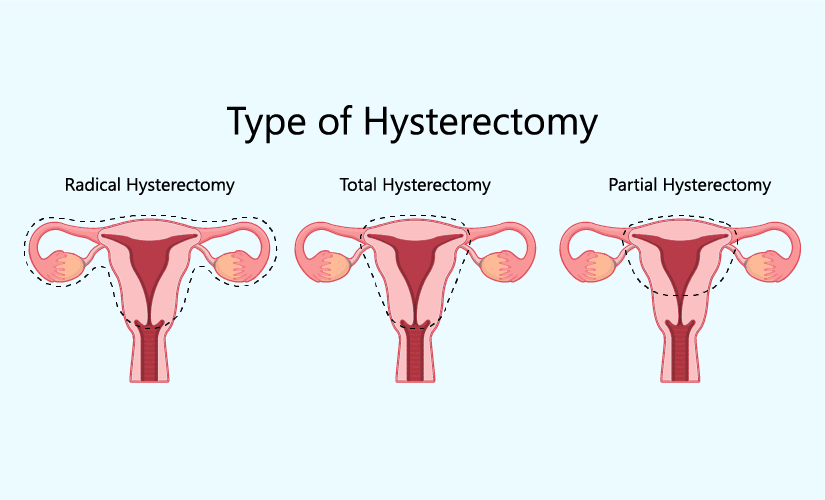
Partial (Subtotal) Hysterectomy: A partial or subtotal hysterectomy involves the removal of the upper part of the uterus while leaving the cervix intact. This procedure is often chosen when the cervix is healthy and does not need to be removed. By preserving the cervix, some of the structural support for the pelvic organs is maintained, potentially reducing the risk of prolapse.
Total Hysterectomy: A total hysterectomy involves the complete removal of both the uterus and the cervix. This is the most common type of hysterectomy and is often performed for conditions such as uterine fibroids, endometriosis, or gynecologic cancers. Removing the cervix eliminates the risk of cervical cancer but may affect the structural support of the pelvic organs.
Radical Hysterectomy: A radical hysterectomy is a more extensive procedure that involves the removal of the uterus, cervix, the upper part of the vagina, and the surrounding tissues, including the parametrium and pelvic lymph nodes. This type of hysterectomy is typically performed for invasive gynecologic cancers, such as cervical or uterine cancer, to ensure the complete removal of cancerous tissues and reduce the risk of recurrence. The procedure may also involve the removal of the ovaries and fallopian tubes.
Laparoscopic and Robotic-Assisted Hysterectomy: Minimally invasive techniques, such as laparoscopic and robotic-assisted hysterectomy, can be used for partial, total, or radical hysterectomies. These approaches involve small incisions and the use of specialized instruments, including a laparoscope or robotic arms, to perform the surgery. These techniques offer the benefits of reduced postoperative pain, shorter hospital stays, and quicker recovery times compared to traditional open surgery.
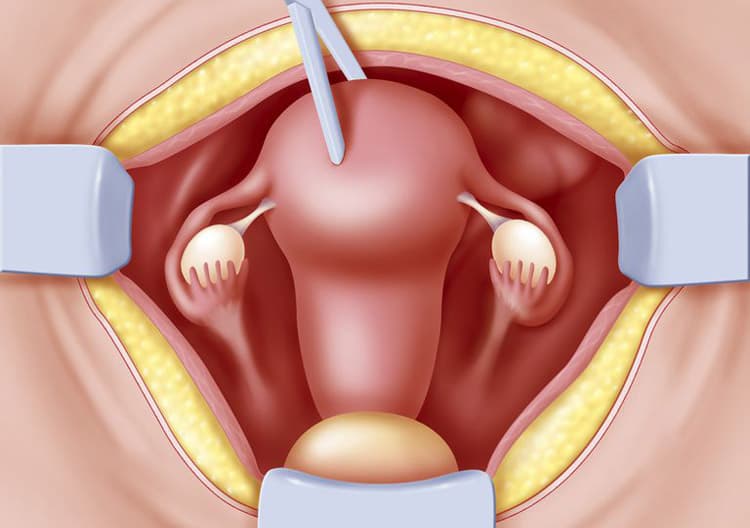
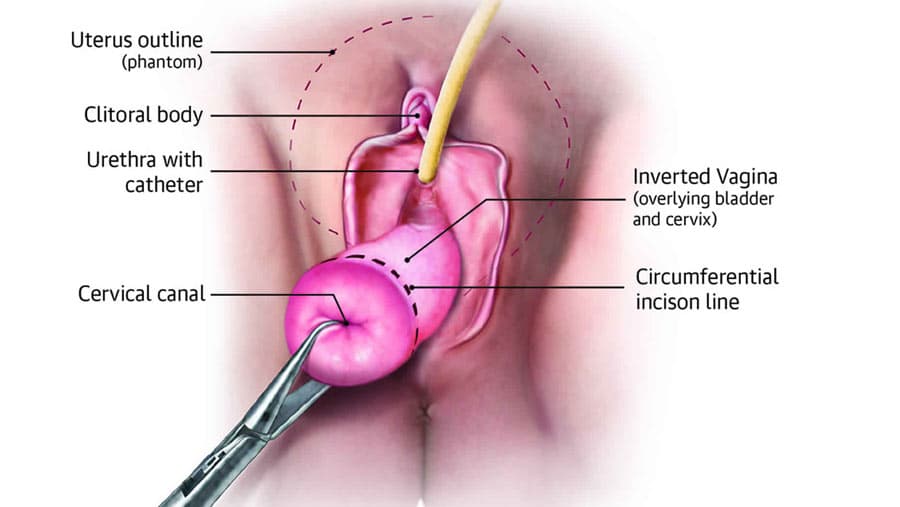
Vaginal Hysterectomy: In a vaginal hysterectomy, the uterus is removed through an incision made in the vagina, with no external incisions. This approach is often used for conditions such as uterine prolapse or when the uterus is not excessively enlarged. Vaginal hysterectomy is associated with less postoperative pain and faster recovery compared to abdominal hysterectomy.
The choice of hysterectomy type depends on factors such as the patient's medical condition, the extent of the disease, and the surgeon's expertise. Each approach has its advantages and potential risks, and careful consideration is essential to achieve the best possible outcomes.
What are Surgical Techniques for Hysterectomy?
There are several surgical techniques for performing a hysterectomy, each designed to address specific medical conditions and patient needs. The choice of technique depends on factors such as the patient's overall health, the underlying condition, the size and position of the uterus, and the surgeon's expertise. The primary surgical techniques for hysterectomy include abdominal, vaginal, laparoscopic, and robotic-assisted approaches.
Abdominal Hysterectomy: An abdominal hysterectomy involves making a horizontal or vertical incision in the lower abdomen to access and remove the uterus. This technique is often used when the uterus is large, there is a need to explore the pelvic region, or there are other complicating factors such as extensive adhesions or endometriosis. Abdominal hysterectomy provides the surgeon with a clear view of the pelvic organs, but it is associated with a longer recovery time, increased postoperative pain, and a higher risk of complications compared to less invasive techniques.
Vaginal Hysterectomy: A vaginal hysterectomy involves removing the uterus through an incision made in the vagina, with no external incisions. This approach is often used for conditions such as uterine prolapse or when the uterus is not excessively enlarged. Vaginal hysterectomy is associated with less postoperative pain, shorter hospital stays, and quicker recovery times compared to abdominal hysterectomy. However, it may not be suitable for patients with large fibroids, extensive endometriosis, or other complicating factors.
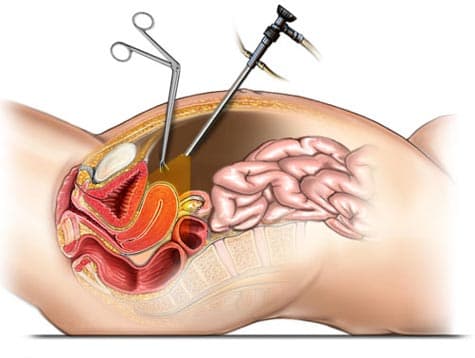
Laparoscopic Hysterectomy: Laparoscopic hysterectomy is a minimally invasive technique that involves making small incisions in the abdomen to insert a laparoscope (a thin, lighted tube with a camera) and specialized surgical instruments. The surgeon uses the laparoscope to visualize the pelvic organs and remove the uterus. This technique offers the benefits of reduced postoperative pain, shorter hospital stays, and quicker recovery times. Laparoscopic hysterectomy can be used for partial, total, or radical hysterectomies and is suitable for a wide range of conditions.
Robotic-Assisted Hysterectomy: Robotic-assisted hysterectomy is a variation of laparoscopic hysterectomy that involves the use of a robotic surgical system to perform the procedure. The surgeon controls the robotic arms from a console, allowing for precise movements and improved visualization of the surgical site. This technique offers the same benefits as traditional laparoscopic hysterectomy, including reduced postoperative pain and quicker recovery times. Robotic-assisted hysterectomy can be especially useful for complex cases, such as those involving extensive adhesions or endometriosis.
What are risks of Hysterectomy?
A hysterectomy, while often necessary for treating various medical conditions, carries several risks and potential complications.
One of the most common risks associated with this surgery is infection, which can occur at the incision sites or within the pelvic cavity. Infections can delay recovery and may require antibiotic treatment or additional surgical intervention.
Bleeding during or after the procedure is another risk, and in some cases, may necessitate blood transfusions or further surgical procedures to control hemorrhage.
Additionally, injury to surrounding organs, such as the bladder, ureters, or intestines, can occur during the surgery, potentially leading to complications that require further medical attention.
Anesthesia-related risks are also a concern, as with any major surgical procedure. Patients may experience adverse reactions to anesthesia, including respiratory issues, allergic reactions, or cardiovascular complications. Blood clots, particularly in the legs (deep vein thrombosis) or lungs (pulmonary embolism), are another potential risk, especially during the postoperative period when mobility is reduced. Measures such as early ambulation, compression stockings, and anticoagulant medications are often used to minimize this risk.
Hormonal changes are a significant consideration, particularly if the ovaries are removed during the hysterectomy (a procedure known as oophorectomy). The removal of the ovaries results in immediate menopause, which can lead to symptoms such as hot flashes, night sweats, mood swings, and an increased risk of osteoporosis and cardiovascular disease. Hormone replacement therapy (HRT) may be recommended to manage these symptoms and reduce long-term health risks.
Long-term complications can include pelvic organ prolapse, where the pelvic organs (such as the bladder or rectum) descend into the vaginal canal due to weakened pelvic floor muscles. This condition can cause discomfort, urinary or bowel issues, and may require further surgical intervention. Additionally, patients may experience changes in sexual function, including decreased libido, vaginal dryness, or pain during intercourse.
Hysterectomy Pros and Cons
A hysterectomy, the surgical removal of the uterus, offers several potential benefits and drawbacks that women must consider before deciding to undergo the procedure. One of the primary advantages of a hysterectomy is the relief from chronic symptoms associated with various gynecological conditions, such as uterine fibroids, endometriosis, chronic pelvic pain, and abnormal bleeding. By removing the source of these symptoms, a hysterectomy can significantly improve a woman's quality of life, allowing her to engage in daily activities without discomfort or pain. Additionally, for women with gynecologic cancers, such as cervical, uterine, or ovarian cancer, a hysterectomy can be a life-saving procedure that removes cancerous tissues and reduces the risk of cancer recurrence.
Another benefit of a hysterectomy is the elimination of menstrual periods, which can be advantageous for women who experience heavy or irregular bleeding that negatively impacts their health and well-being. The procedure also removes the risk of uterine and cervical cancers, providing peace of mind for women at high risk for these conditions.
However, a hysterectomy also has several potential drawbacks. One of the main concerns is the loss of fertility, as the removal of the uterus means that a woman can no longer conceive or carry a pregnancy. This can be a significant consideration for women who desire to have children in the future. Additionally, if the ovaries are removed during the procedure (oophorectomy), it can result in immediate menopause, leading to symptoms such as hot flashes, night sweats, mood swings, and an increased risk of osteoporosis and cardiovascular disease. Hormone replacement therapy (HRT) may be required to manage these symptoms and reduce long-term health risks.
Other potential risks and complications of a hysterectomy include infection, bleeding, injury to surrounding organs (such as the bladder, ureters, or intestines), and anesthesia-related complications. Long-term issues may include pelvic organ prolapse, where the pelvic organs descend into the vaginal canal due to weakened pelvic floor muscles, and changes in sexual function, such as decreased libido, vaginal dryness, or pain during intercourse.
Recovering from a hysterectomy
Recovering from a hysterectomy is a process that requires time, patience, and careful management to ensure the best possible outcomes for patients. The recovery period varies depending on the type of hysterectomy performed, the surgical technique used, and the individual's overall health. Immediately after the surgery, patients are taken to a recovery area where healthcare professionals closely monitor their vital signs, manage pain, and address any immediate complications. The initial hospital stay can range from one to several days, depending on the surgical approach and the patient's condition.
Pain management is a crucial aspect of recovery, and patients may receive medications to control discomfort and enable them to engage in gentle physical activity, such as walking, to promote circulation and prevent blood clots. Gradually increasing physical activity is essential to regain strength and improve overall well-being. Patients should avoid heavy lifting, strenuous exercise, and activities that strain the abdominal muscles for several weeks to allow the surgical site to heal properly.
Nutritional support is also important during the recovery process. A balanced diet rich in nutrients can aid in healing and improve energy levels. Patients may be advised to avoid certain foods that can cause bloating or constipation and to drink plenty of fluids to stay hydrated.
Emotional and mental well-being is another critical component of recovery. Patients may experience a range of emotions, including relief, sadness, or anxiety, as they adjust to the changes in their body and reproductive health. Seeking support from family, friends, or support groups can help patients navigate these emotions and cope with the recovery process.
Regular follow-up appointments with healthcare providers are essential to monitor progress, address any concerns, and make necessary adjustments to the recovery plan. Healthcare professionals will assess the healing process, check for any complications, and provide guidance on resuming normal activities.
Conclusion
In conclusion, a hysterectomy is a significant surgical procedure that offers relief from various debilitating gynecological conditions and can be life-saving for women with gynecologic cancers. While it carries potential risks and long-term consequences, the benefits of alleviating chronic pain, abnormal bleeding, and other symptoms often outweigh these challenges. The decision to undergo a hysterectomy requires careful consideration, thorough evaluation by healthcare professionals, and a comprehensive understanding of the procedure's impact on physical and emotional well-being. With appropriate preoperative preparation, skilled surgical techniques, and diligent postoperative care, many women experience improved quality of life and relief from the conditions that necessitated the surgery. Regular follow-up and support are essential to ensure a successful recovery and to address any concerns that may arise during the healing process.
Read More