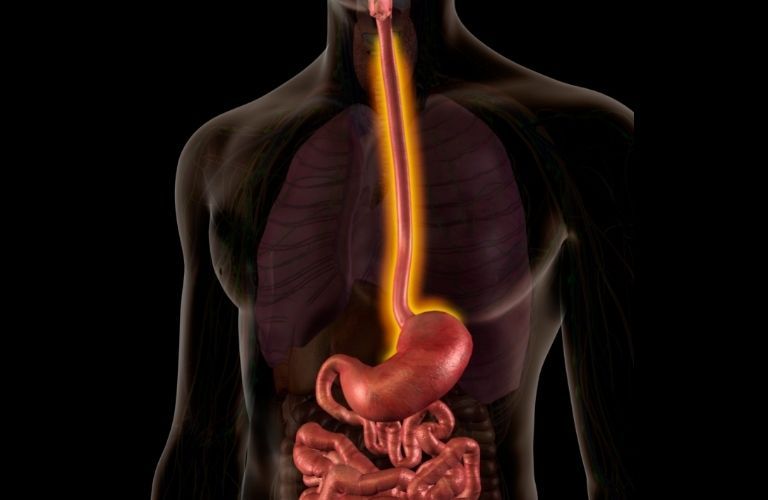
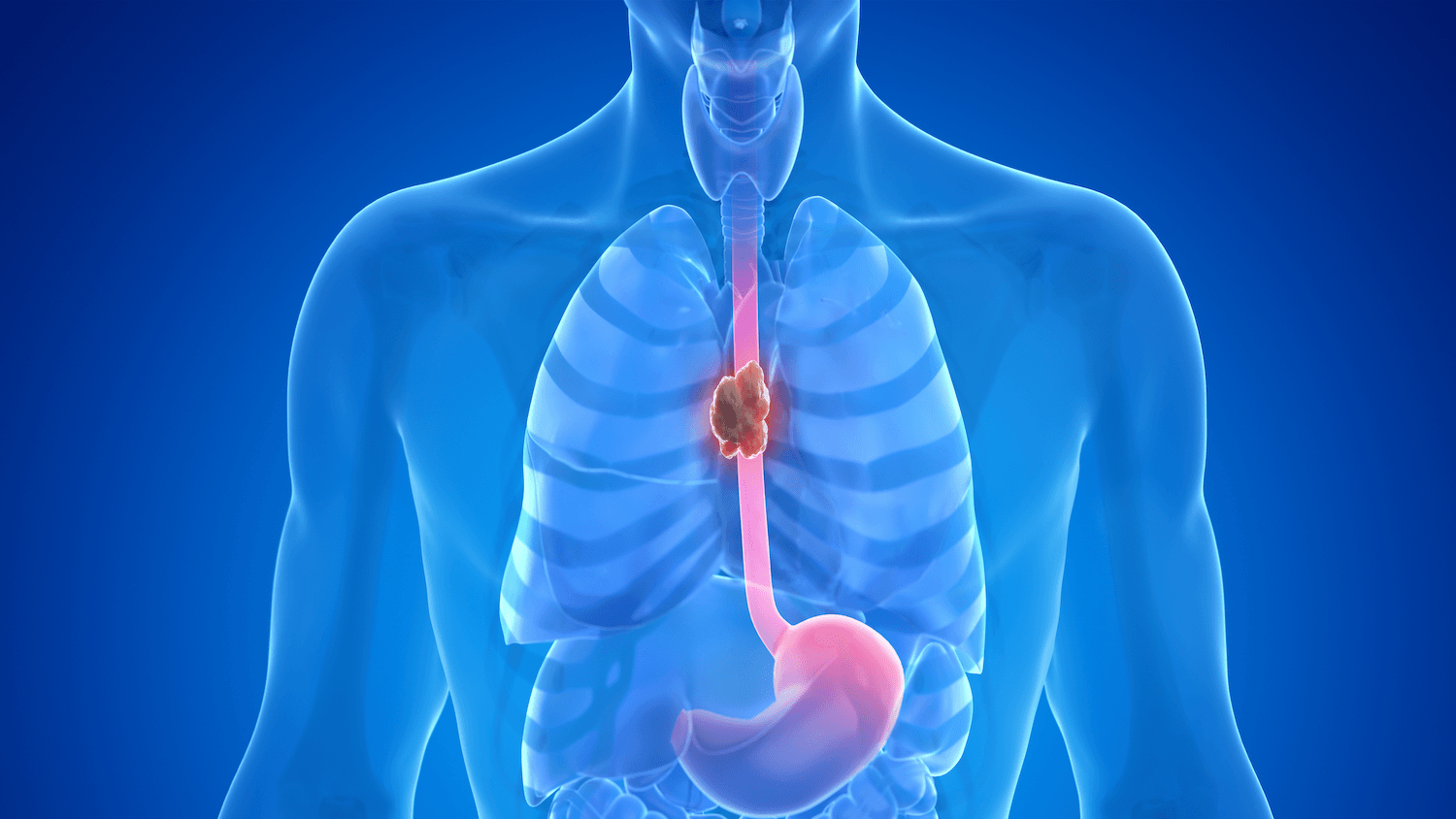
Esophagectomy is a surgical procedure that involves the removal of all or part of the esophagus, which is the muscular tube that connects the throat to the stomach. This surgery is typically performed to treat esophageal cancer, but it may also be used to address other conditions such as severe esophageal strictures, Barrett's esophagus with high-grade dysplasia, or esophageal motility disorders that do not respond to other treatments.
What are the Types of esophagectomy?
There are several types of esophagectomy, each tailored to the specific needs of the patient and the location and extent of the disease. The three main types of esophagectomy are as follows.
Transhiatal Esophagectomy (THE)
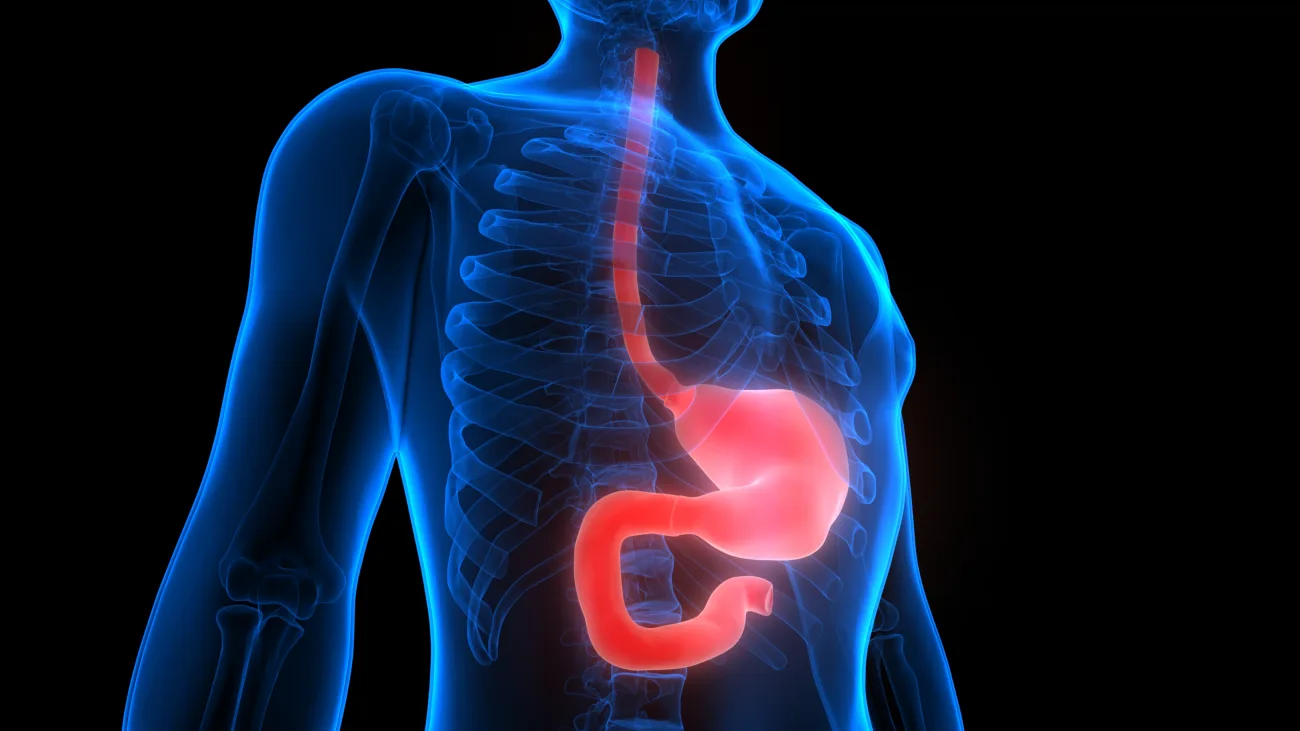
Transhiatalesophagectomyinvolves the removal of the esophagus through two main incisions—one in the neck and one in the upper abdomen. This approach avoids the need for a thoracic (chest) incision. The surgeon removes the affected portion of the esophagus and then pulls up the stomach to connect it to the remaining esophagus in the neck. This technique is often used for tumors located in the lower part of the esophagus and for patients who may not tolerate a thoracotomy (chest incision) well. THE can reduce postoperative pain and shorten recovery time, but it may not be suitable for all patients, especially those with extensive disease.
Transthoracic Esophagectomy (TTE)
Transthoracic esophagectomy involves the removal of the esophagus through an incision in the chest. There are two main variations of TTE: the Ivor Lewis esophagectomy and the three-incision esophagectomy. The Ivor Lewis esophagectomy involves an abdominal incision and a right thoracic incision, while the three-incision esophagectomy involves additional cervical (neck) incision. The surgeon removes the diseased esophagus and reconstructs the digestive tract by pulling up the stomach or using a segment of the intestine. TTE allows for a more thorough removal of the esophagus and lymph nodes, making it suitable for patients with more extensive disease. However, it is a more complex procedure and may involve a longer recovery period.
Minimally Invasive Esophagectomy (MIE)
Minimally invasive esophagectomy is performed using small incisions and specialized instruments, including a laparoscope and thoracoscope. This approach can be used for both transhiatal and transthoracic techniques, depending on the patient's condition. MIE offers the benefits of reduced postoperative pain, shorter hospital stays, and quicker recovery times compared to traditional open surgery. It also allows for precise surgical techniques and improved visualization. However, MIE requires specialized training and expertise, and not all patients are suitable candidates for this approach.

How to prepare for Esophagectomy?
Preparing for anesophagectomyinvolves several important steps to ensure the best possible outcomes and a smooth recovery. The preparation process typically begins with a thorough evaluation by a multidisciplinary team of healthcare professionals, including surgeons, anesthesiologists, and nutritionists. They will assess the patient's overall health, medical history, and the extent of the esophageal condition to determine the most appropriate surgical approach and plan.
One of the key aspects of preparation is optimizing the patient's physical condition. This may involve quitting smoking, as smoking can impair lung function and increase the risk of complications during and after surgery. Patients are also encouraged to engage in regular physical activity to improve their cardiovascular fitness and overall strength. A balanced diet rich in nutrients is essential to support the body's healing processes. In some cases, patients may need to undergo nutritional counseling to ensure they are adequately nourished before the surgery.
Patients will also undergo a series of preoperative tests and imaging studies, such as blood tests, chest X-rays, and CT scans, to evaluate their overall health and the specific characteristics of their esophageal condition. These tests help the surgical team plan the procedure and anticipate any potential challenges.
Mental and emotional preparation is equally important. Patients should discuss their concerns and expectations with their healthcare team and seek support from family, friends, or support groups. Understanding the procedure, potential risks, and the recovery process can help alleviate anxiety and build confidence in the surgical plan.
Patients should also follow their surgeon's preoperative instructions carefully. This may include fasting for a certain period before the surgery, stopping certain medications, and taking prescribed preoperative medications as directed. It is important to arrange for postoperative care, such as transportation home from the hospital and assistance with daily activities during the initial recovery period.

What happens during an Esophagectomy?
During an esophagectomy, the surgeon removes all or part of the esophagus, the muscular tube that carries food from the throat to the stomach. The procedure typically begins with the patient under general anesthesia to ensure they are comfortable and pain-free throughout the surgery. The specific surgical approach may vary depending on the patient's condition and the surgeon's preference, but the three main types of esophagectomy are transhiatal, transthoracic, and minimally invasive esophagectomy.
In a transhiatal esophagectomy, the surgeon makes an incision in the neck and another in the upper abdomen, avoiding the need for a chest incision. The diseased portion of the esophagus is removed, and the stomach is pulled up to connect with the remaining esophagus in the neck. In a transthoracic esophagectomy, the surgeon makes an incision in the chest, along with abdominal and sometimes neck incisions. This approach allows for a more thorough removal of the esophagus and nearby lymph nodes, which is often necessary for more extensive disease. In a minimally invasive esophagectomy, the surgeon uses small incisions and specialized instruments, including a laparoscope and thoracoscope, to perform the procedure. This technique offers the benefits of reduced postoperative pain, shorter hospital stays, and quicker recovery times.
Once the diseased portion of the esophagus is removed, the surgeon reconstructs the digestive tract to restore continuity between the throat and the stomach. This is usually achieved by pulling up the stomach to create a new connection, although in some cases, a segment of the intestine may be used. The surgeon then ensures that the new connection is secure and functional, and drains are often placed to remove any excess fluid that may accumulate during the healing process.
Throughout the procedure, the patient's vital signs are closely monitored to ensure their safety. After the surgery is complete, the patient is moved to the recovery room and eventually to an intensive care unit (ICU) for close observation. The recovery process involves managing pain, preventing complications, and gradually reintroducing oral intake to ensure the patient's digestive system functions properly.
What Are Common Esophagectomy Complications?
Esophagectomy, while potentially life-saving, is a complex surgical procedure that carries several common complications. In the immediate postoperative period, patients may experience pain, swelling, and discomfort at the incision sites, which are managed with pain medications.
One of the significant risks associated with esophagectomy is the potential for anastomotic leaks, where the new connection between the remaining esophagus and stomach (or intestine) does not heal properly, leading to leakage of gastric contents. This can result in severe infection, sepsis, and the need for additional surgical interventions. Respiratory complications, such as pneumonia and respiratory failure, are also common due to the proximity of the esophagus to the lungs and the impact of surgery on breathing.
Infection at the incision sites or within the chest cavity is another potential complication that can delay recovery and require antibiotic treatment. Bleeding during or after the surgery is a risk, and in some cases, may necessitate blood transfusions or further surgical intervention. Prolonged air leaks and pleural effusions, where excess fluid accumulates around the lungs, can occur and may require drainage procedures.
Patients may also experience long-term complications following an esophagectomy. Stricture formation, where scar tissue narrows the newly constructed esophagus, can lead to swallowing difficulties and may require dilation procedures to widen the esophagus. Nutritional deficiencies are a concern, as changes in the digestive system can affect the absorption of nutrients. Patients may need to adopt specific dietary adjustments and take supplements to maintain their nutritional status.
The recovery process following an esophagectomy is lengthy and requires close monitoring and support from healthcare professionals. While the risks and complications are significant, the potential benefits of an esophagectomy, such as the removal of cancerous or diseased tissue and improved quality of life, often outweigh these challenges for carefully selected patients. Regular follow-up appointments are essential to detect and manage any complications promptly and to ensure the best possible outcomes for the patient.
Esophagectomy Recovery
Recovering from an esophagectomy is a multi-faceted process that involves close monitoring, rehabilitation, and support to ensure optimal outcomes for patients. The initial phase of recovery typically occurs in the hospital, where patients are closely observed by a multidisciplinary team of healthcare professionals, including surgeons, nurses, and respiratory therapists. This team manages pain, monitors vital signs, and addresses any immediate complications. Patients may be placed in an intensive care unit (ICU) for the first few days to ensure they receive the highest level of care. During this time, they may require supplemental oxygen and specialized breathing exercises to help their lungs recover and regain strength.
Pain management is crucial during the recovery process. Patients receive medications to control discomfort, which enables them to participate in rehabilitation activities and engage in gentle physical activity, such as walking, to promote lung expansion and prevent blood clots. Nutritional support is also essential, as patients may initially receive nutrition through a feeding tube while their digestive system heals. Gradually, they transition to a liquid diet and then to soft foods as tolerated.
Once discharged from the hospital, patients continue their recovery at home, often with the support of a pulmonary rehabilitation program. These programs are designed to help patients gradually increase their physical activity levels, improve lung function, and enhance overall endurance. Pulmonary rehabilitation typically includes supervised exercise sessions, breathing techniques, and education on managing esophageal conditions.
The recovery process can take several months, and patients must be patient and committed to following their rehabilitation plan. Regular follow-up appointments with healthcare providers are essential to monitor progress, address any concerns, and make necessary adjustments to the treatment plan. Patients are also advised to adopt a healthy lifestyle, including smoking cessation, a balanced diet, and regular exercise, to maintain the benefits of the surgery and prevent further health issues.
While the recovery from an esophagectomy can be challenging, many patients experience significant improvements in their quality of life, including better swallowing function, increased physical activity levels, and reduced symptoms of their underlying esophageal condition. The support of healthcare professionals, family, and friends plays a vital role in helping patients navigate the recovery journey and achieve the best possible outcomes.
Conclusion
In conclusion, esophagectomy is a complex and potentially life-saving surgical procedure primarily used to treat esophageal cancer and other severe esophageal conditions. By removing the diseased or damaged portion of the esophagus and reconstructing the digestive tract, esophagectomy can significantly improve a patient's quality of life and offer a chance for long-term survival. While the surgery carries risks and requires a lengthy recovery period, careful patient selection, meticulous surgical techniques, and comprehensive postoperative care can help minimize complications and enhance outcomes. With the support of a multidisciplinary healthcare team, patients undergoing esophagectomy can navigate the challenges of recovery and work towards achieving a healthier, more fulfilling life.
Read More