Cerebrovascular diseases encompass a range of medical conditions that affect the blood vessels and blood supply to the brain. These conditions are primarily caused by impaired circulation within the brain's vascular system, leading to a reduction or complete blockage of blood flow to certain areas of the brain.
What blood vessels do cerebrovascular diseases affect?
Cerebrovascular diseases primarily affect the blood vessels that supply blood to the brain, including the carotid and vertebral arteries. These blood vessels play a crucial role in delivering oxygen and essential nutrients to brain tissues, ensuring proper neurological function and overall brain health.
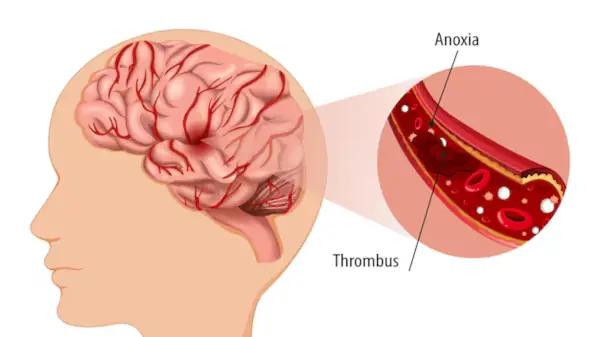
The carotid arteries are a pair of major blood vessels located on each side of the neck. They branch from the aorta, the body's main artery, and ascend to the base of the skull, where they further divide into the internal and external carotid arteries. The internal carotid arteries are particularly important as they supply blood to the anterior (front) part of the brain, including critical areas responsible for motor and sensory functions, language, and cognitive processes. Cerebrovascular diseases affecting the carotid arteries, such as carotid artery stenosis, involve the narrowing or blockage of these vessels due to the buildup of atherosclerotic plaques. This can lead to reduced blood flow to the brain and increase the risk of ischemic stroke, where a blood clot obstructs blood supply to a specific brain region, resulting in brain tissue damage.
The vertebral arteries are also essential contributors to cerebral blood flow. They originate from the subclavian arteries, which arise from the aorta, and travel along the cervical spine (neck vertebrae) before merging to form the basilar artery at the base of the brain. The vertebral arteries supply blood to the posterior (back) part of the brain, including the brainstem, cerebellum, and occipital lobes. These regions are responsible for vital functions such as balance, coordination, vision, and basic life-sustaining activities like breathing and heart rate regulation. Cerebrovascular diseases affecting the vertebral arteries can lead to vertebrobasilar insufficiency, where reduced blood flow causes symptoms such as dizziness, vertigo, and vision problems. Severe cases can result in ischemic strokes affecting the posterior circulation of the brain.
Both the carotid and vertebral arteries can be affected by various risk factors, including hypertension, diabetes, high cholesterol, smoking, and obesity. Managing these risk factors through lifestyle modifications, medications, and regular medical check-ups is essential to prevent the progression of cerebrovascular diseases. Early detection and intervention, such as carotid endarterectomy or angioplasty for carotid artery stenosis, can significantly reduce the risk of stroke and improve outcomes for patients with cerebrovascular conditions.
What are the types of cerebrovascular diseases?
Cerebrovascular diseases encompass a wide range of medical conditions that affect the blood vessels and blood supply to the brain, leading to significant neurological damage and potentially life-threatening consequences. Understanding the various types of cerebrovascular diseases is crucial for early detection, prevention, and effective treatment.
One of the most well-known cerebrovascular diseases is stroke, which can be classified into two main types: ischemic stroke and hemorrhagic stroke. Ischemic strokes account for approximately 85% of all strokes and occur when a blood clot obstructs blood flow to a specific area of the brain. This can happen due to the buildup of atherosclerotic plaques in the carotid or vertebral arteries, leading to a condition known as carotid artery stenosis. Hemorrhagic strokes, on the other hand, result from the rupture of a blood vessel within the brain, causing bleeding and increased pressure on brain tissues. Hemorrhagic strokes can be further divided into intracerebral hemorrhages, which occur within the brain tissue, and subarachnoid hemorrhages, which occur in the space between the brain and the surrounding membranes.
Transient ischemic attacks (TIAs), often referred to as "mini-strokes," are another type of cerebrovascular disease. TIAs are temporary episodes of impaired blood flow to the brain that cause stroke-like symptoms but do not result in permanent damage. TIAs serve as important warning signs for an impending stroke and require prompt medical attention to prevent a full-blown stroke.
Cerebral aneurysms are another significant cerebrovascular condition. An aneurysm is a weakened area in the wall of a blood vessel that can balloon out and potentially rupture, leading to a hemorrhagic stroke. Aneurysms can develop in any blood vessel within the brain, but they are most commonly found in the arteries at the base of the brain, known as the Circle of Willis.
Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels that can disrupt normal blood flow and oxygen circulation in the brain. AVMs can lead to bleeding within the brain, seizures, and other neurological symptoms. Early detection and management of AVMs are essential to prevent severe complications.
Other cerebrovascular diseases include cerebral venous sinus thrombosis (CVST), a rare condition where blood clots form in the brain's venous sinuses, leading to increased intracranial pressure and potential brain damage. Moyamoya disease is a progressive condition characterized by the narrowing of cerebral arteries, leading to the development of fragile collateral vessels that can rupture and cause hemorrhagic strokes.
Understanding the different types of cerebrovascular diseases is vital for promoting brain health and preventing the devastating effects of impaired blood flow to the brain. Advances in medical research and technology continue to improve our ability to diagnose, treat, and manage these conditions, offering hope for better outcomes and enhanced quality of life for affected individuals.

What causes cerebrovascular disease?
Cerebrovascular diseases, which impact the blood vessels and blood supply to the brain, can arise from various underlying causes and risk factors.
One of the primary contributors to cerebrovascular disease is atherosclerosis, a condition characterized by the buildup of fatty deposits (plaques) along the inner walls of arteries. These plaques can narrow or block the arteries, reducing blood flow to the brain and increasing the risk of ischemic stroke. Hypertension, or high blood pressure, is another significant risk factor. Elevated blood pressure can damage the blood vessel walls over time, making them more susceptible to atherosclerosis, aneurysms, and hemorrhagic strokes.
Diabetes is also a major cause of cerebrovascular diseases. Individuals with diabetes are at higher risk due to the damaging effects of elevated blood sugar levels on blood vessels, which can lead to atherosclerosis and other vascular complications. High cholesterol levels contribute to the formation of plaques in the arteries, further exacerbating the risk of cerebrovascular disease. Smoking is a well-documented risk factor as well; the harmful chemicals in tobacco smoke damage blood vessel walls and promote the buildup of plaques.
Obesity and a sedentary lifestyle are additional contributors. Excess body weight and physical inactivity can lead to conditions such as hypertension, diabetes, and high cholesterol, all of which elevate the risk of cerebrovascular diseases. Genetic predisposition also plays a role, as individuals with a family history of stroke or other vascular conditions may be more susceptible.
Moreover, certain medical conditions and lifestyle factors can lead to specific types of cerebrovascular disease. For example, atrial fibrillation, a type of irregular heartbeat, increases the risk of blood clots forming in the heart, which can travel to the brain and cause an ischemic stroke. Excessive alcohol consumption and drug use can contribute to the development of conditions like aneurysms or hemorrhagic strokes.

How is cerebrovascular disease diagnosed?
Diagnosing cerebrovascular disease involves a combination of medical history evaluation, physical examinations, and advanced imaging techniques to accurately assess the condition and determine the appropriate course of treatment.
The diagnostic process typically begins with a detailed medical history, where the healthcare provider inquiries about the patient's symptoms, risk factors, and family history of cerebrovascular conditions. This information helps identify potential underlying causes and guides further diagnostic testing.
During the physical examination, the healthcare provider assesses the patient's neurological function, checking for signs of weakness, numbness, speech difficulties, or other neurological deficits that may indicate cerebrovascular disease. The examination may also include blood pressure measurements and evaluations of the heart and blood vessels to identify any contributing factors.
Advanced imaging techniques play a crucial role in diagnosing cerebrovascular disease. One of the most commonly used imaging methods is computed tomography (CT) scanning, which provides detailed cross-sectional images of the brain, helping to identify areas of bleeding, infarction (tissue death due to lack of blood flow), or other abnormalities. Magnetic resonance imaging (MRI) is another powerful tool that offers high-resolution images of brain structures and can detect early signs of cerebrovascular disease, such as small strokes or transient ischemic attacks (TIAs).
In addition to these imaging techniques, vascular imaging methods are often employed to visualize the blood vessels in and around the brain. Carotid ultrasound, for example, uses sound waves to create images of the carotid arteries in the neck, allowing healthcare providers to assess for narrowing or blockages. Magnetic resonance angiography (MRA) and computed tomography angiography (CTA) provide detailed images of the brain's blood vessels, helping to identify aneurysms, arteriovenous malformations (AVMs), or other vascular abnormalities.
Other diagnostic tests may include blood tests to evaluate cholesterol levels, blood sugar levels, and markers of inflammation, as well as electrocardiograms (ECGs) to assess heart rhythm and function. Together, these diagnostic tools provide a comprehensive understanding of the patient's cerebrovascular health, enabling healthcare providers to develop an effective treatment plan to manage and prevent further complications.

How is cerebrovascular disease treated?
Treatment of cerebrovascular disease focuses on restoring adequate blood flow to the brain, preventing further complications, and managing underlying risk factors. The approach to treatment depends on the specific type of cerebrovascular disease, its severity, and the patient's overall health.
For ischemic stroke, which is caused by a blood clot obstructing blood flow to the brain, the primary treatment involves the use of thrombolytic (clot-busting) medications such as tissue plasminogen activator (tPA). Administered intravenously within a critical time window (usually within 3 to 4.5 hours of symptom onset), tPA can dissolve the clot and restore blood flow, reducing the extent of brain damage. In some cases, mechanical thrombectomy, a minimally invasive procedure, may be performed to physically remove the clot using a catheter-based device.
Hemorrhagic stroke, resulting from a ruptured blood vessel causing bleeding in the brain, requires different treatment strategies. The focus is on controlling the bleeding and reducing intracranial pressure. This may involve surgical intervention to repair the damaged blood vessel, such as clipping or coiling an aneurysm or removing a hematoma (accumulated blood). Medications to manage blood pressure, prevent seizures, and control brain swelling are also commonly used.
Preventive measures are crucial for managing cerebrovascular disease and reducing the risk of recurrent strokes or other complications. Lifestyle modifications, including adopting a heart-healthy diet, regular physical activity, smoking cessation, and limiting alcohol consumption, are essential.
Surgical procedures, such as carotid endarterectomy or carotid artery stenting, may be recommended for patients with significant carotid artery stenosis to remove or bypass the plaque causing the blockage.
Rehabilitation is a critical component of treatment for patients recovering from a stroke or other cerebrovascular event. Physical therapy, occupational therapy, and speech therapy help patients regain lost functions, improve mobility, and enhance their quality of life.
How can I reduce my risk of cerebrovascular disease?
Reducing the risk of cerebrovascular disease involves adopting a healthy lifestyle and managing key risk factors that contribute to the development of these conditions.
One of the most important steps you can take is to maintain a heart-healthy diet. This includes consuming plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats such as those found in nuts, seeds, and olive oil. Limiting the intake of saturated fats, trans fats, sodium, and added sugars can help keep your blood pressure and cholesterol levels in check, reducing the risk of atherosclerosis and other vascular problems.
Regular physical activity is another crucial component in preventing cerebrovascular disease. Aim for at least 150 minutes of moderate-intensity aerobic exercise, such as brisk walking, cycling, or swimming, each week. Exercise helps improve cardiovascular health, lower blood pressure, and maintain a healthy weight, all of which are essential for reducing the risk of stroke and other cerebrovascular conditions.
Avoiding tobacco use is vital, as smoking significantly damages blood vessels and increases the risk of stroke. If you smoke, seek support to quit, and avoid exposure to secondhand smoke. Limiting alcohol consumption is also important, as excessive drinking can raise blood pressure and contribute to other risk factors. Stick to moderate drinking guidelines, which generally recommend no more than one drink per day for women and two drinks per day for men.
Managing chronic health conditions, such as hypertension, diabetes, and high cholesterol, is essential for reducing the risk of cerebrovascular disease. Regular check-ups with your healthcare provider can help monitor these conditions and ensure they are well-controlled. Medications may be prescribed to manage blood pressure, blood sugar levels, and cholesterol, and it's important to take them as directed.
Stress management techniques, such as mindfulness, meditation, and relaxation exercises, can also be beneficial. Chronic stress can negatively impact cardiovascular health, so finding healthy ways to cope with stress is important for overall well-being.
By adopting these lifestyle changes and working closely with your healthcare provider, you can significantly reduce your risk of cerebrovascular disease and promote better brain and cardiovascular health.

Conclusion
In conclusion, cerebrovascular diseases represent a significant medical challenge, encompassing a variety of conditions that affect the blood vessels and blood supply to the brain. These diseases, including strokes, transient ischemic attacks (TIAs), aneurysms, and arteriovenous malformations (AVMs), can lead to severe neurological damage and life-threatening complications. Understanding the underlying causes, recognizing the symptoms, and seeking timely medical intervention are crucial for effective management and prevention. Advances in medical research and technology have improved our ability to diagnose and treat cerebrovascular diseases, offering hope for better outcomes and enhanced quality of life for affected individuals. By adopting a healthy lifestyle, managing risk factors, and staying vigilant about cerebrovascular health, individuals can significantly reduce their risk and promote overall brain and cardiovascular well-being.
Read More