Liver transplant surgery is a life-saving procedure that replaces a diseased and failing liver with a healthy one. Those on the waiting list for a new liver usually have end-stage liver disease, acute liver failure, or liver cancer. Those who receive liver transplants are critically ill with no other treatment option. The liver, as the largest internal organ performs several critical functions including:
Processing nutrients, medications, and hormones
Producing bile, which helps the body absorb fats, cholesterol, and fat-soluble vitamins
Making proteins that help the blood clot
Removing bacteria and toxins from the blood
Preventing infection and regulating immune responses
An alternative to waiting for a deceased donor's liver to become available is receiving a portion of a liver from a living donor. Living-donor liver transplant is possible because the human liver regenerates and returns to its normal size shortly after the surgical removal of part of the organ.

Why is a liver transplant done?
A liver transplant is considered a treatment option for those with liver cancer and those with liver failure whose conditions can no longer be controlled with other treatments. If liver failure happens over a matter of weeks, it’s called acute liver failure. Although a liver transplant may treat acute liver failure, it is more often used to treat chronic liver failure. Chronic liver failure occurs slowly over months and years. The most common cause of chronic liver failure is scarring of the liver (cirrhosis).
Types of Liver transplant
Deceased organ donation: Transplanting liver from a person who died recently
Living donor liver transplant: Transplanting a section of the liver from a living donor (the liver can regenerate itself) – therefore in both the donor and receiver’s body the liver will regrow into a normal-size
Split donation: A liver is removed from a person who died recently and is split into two pieces; each piece is transplanted into a different person, where they will grow to a normal size
Liver transplant requirements
In cases when the liver is no longer functioning properly, a liver transplant is the only option. To be considered for a liver transplant, you must meet certain criteria:
Disease
Your liver must be not functioning properly and beyond the stage that can be repaired. If your liver is damaged, it will grow new tissue to heal itself, but when scarring of the liver occurs (called cirrhosis) it can lead to:
Liver failure
Portal hypertension, where the scarring inhibits blood flow causing pressure to increase in the vein that brings blood to the liver (portal vein)
Hepatocellular carcinoma, or primary liver cancer
Health status
Before you’re considered a viable candidate for a liver transplant, you will need a pre-transplant evaluation, which may include tests such as:
Assessment by a hepatologist (liver specialist)
Assessment by a transplant surgeon
Lab tests, such as blood work, X-rays, and imaging tests like CT or MRI scans
Endoscopy to examine your digestive tract
Colonoscopy to examine your large intestine
Heart and stress tests, such as an electrocardiogram (EKG)
Emotional evaluation to determine your ability to handle stress and follow medical instructions
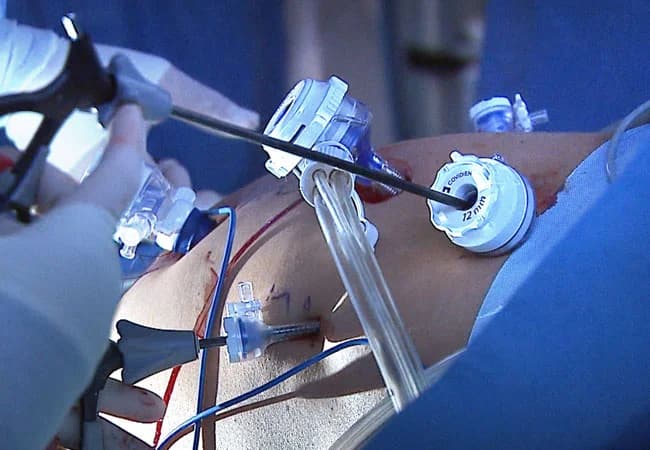
What happens during liver transplant surgery?
As a major surgery, a liver transplant operation takes 6-12 hours. Your surgeon will first make a long incision across your abdomen to access your liver. Then your liver will be carefully separated, then your blood vessels and bile ducts that were connected to them will be clamped. Then they’ll install the new liver and attach it to your blood vessels and bile ducts. After closing your incision, they’ll send you to intensive care.

Conclusion
In conclusion, a liver transplant is a life-saving procedure that has revolutionized the treatment of many liver diseases. It involves the replacement of a diseased liver with a healthy one, often from a deceased donor, but sometimes from a living donor. Despite the complexity of the procedure, advancements in surgical techniques and post-operative care have significantly improved the success rates. However, it’s not without risks and challenges, including organ rejection and long-term dependence on immunosuppressive drugs. Therefore, patients must have a comprehensive understanding of the procedure, its benefits, and potential complications. Continued research and innovation in this field are essential to further improve patient outcomes and quality of life post-transplant.
Read more: