Overview
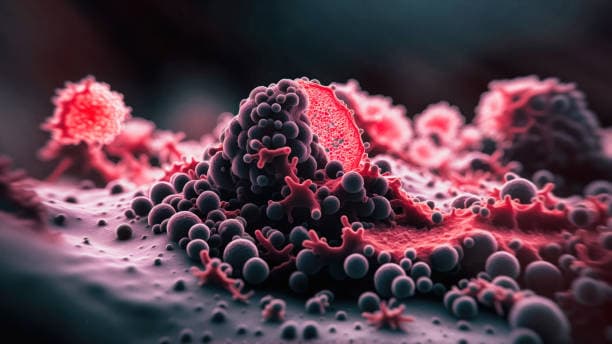
Cancer diagnosis often involves a combination of physical examinations, imaging scans (such as CT, MRI, or PET), blood tests, and biopsies, where tissue samples are examined for cancerous cells. Once diagnosed, treatment plans are tailored to the type and stage of cancer, along with the patient’s overall health. Common treatments include surgery to remove tumors, chemotherapy, radiation therapy, immunotherapy, and targeted therapy, which all aim to eliminate or control the growth of cancer cells and improve the patient’s prognosis.